Episode #114: Drop Acid with Dr. Perlmutter
No, not that acid. Put away your Coachella outfits, folks. Our guest today is neurologist and author Dr. David Perlmutter. His latest book, Drop Acid, is out tomorrow. Inspired by a conversation between Dr. Peter Attia and Dr. Richard Johnson about the impact of Uric Acid on our health, Dr. Perlmutter did a deep dive into the impacts of Uric Acid on our metabolic function. He offers clear, concise takeaways and provides easy-to-understand information. I personally came away with some things to add to my own personal health support to-do list. Enjoy.
Listen to the episode here:
[podcast_subscribe id=”5950″]
Key Topics:
- Brain Health Practices [00:02:50]
- Alzheimer’s and Lifestyle [00:08:11]
- What Inflammation Really Does [00:19:40]
- The Optimal Range [00:33:19]
- Gut Bacteria [00:45:05]
- Supplements to Take Note of [00:56:42]
- Setting an Example [01:00:07]
Drop Acid with Dr. Perlmutter
My guest is neurologist Dr. David Perlmutter. You may know some of his previous books like Grain Brain and Brain Maker. His latest book is out called Drop Acid. It’s not what you think. It’s all about uric acid. A lot of us think of gout or kidney stones and that’s for those kinds of people, but it’s a low-grade inflammation that can impact all of us.
This book was inspired originally, Perlmutter was going on a run and he was listening to a podcast between Dr. Peter Attia, whom I love, and Dr. Richard Johnson. It was all about the overall implications and impact on our health with uric acid. For example, I already take quercetin but after learning some things in this conversation, I’ve upped my intake. He gives a ton of takeaways on ways that we can consider the impact of uric acid. A lot of times, it can just show up as a low-grade inflammation. Dr. Perlmutter is dedicated to helping us navigate better metabolic function. It’s clear, it’s concise. I hope you enjoy.
—
Dr. Perlmutter, before we get into your book, Drop Acid, I was first introduced to you, like a lot of people, from Grain Brain. I read that book. What I’d like to start with is your own practice because I look at you and I see that you live a healthy lifestyle. You even shared some stories inside this book about discovering on a run listening to Peter Attia talk to Dr. Richard Johnson about uric acid and how this book came about.
When people have all this information, civilians think they have it all figured out. In this case, I’ll even put myself in that case, we all feel like civilians, even if we know something about something because we look at other people and we think, “It must be easy for them.” I get the sense that since you were young, I even came across a story about you at 16 years old writing an article, were you born this way? What are some of the practices you have in place to support your own health? Because you’re busy and you have a lot going on. How do you do that?
It paves the way for a sense of transparency moving forward. I’m not a youngster anymore and I am enjoying these years of my life because I’ve made the changes that you’re talking about, which are not easy for me and therefore not easy for others. It’s about bringing the adult into the room and realizing that there’s a big difference between what we want and what we know is better for us.
Our programming is to seek out sweet. Sweet means safe, it means good for us, it means survival. Our ancestors would find berries, eat berries, would make extra fat, and we would survive during times of caloric scarcity. Everybody on the planet has a sweet tooth. It’s about bringing the adult in the room, bringing that part of your brain on board that says, “You want it right now but what’s going to be the long-term play?”
For over three decades of dealing with patients with challenging neurological problems, which are by and large related to their lifestyle choices, and being with my father when he died of Alzheimer’s disease. Watching this beautiful person be ravaged by a disease that is preventable reinforced my need to do this for myself but for my family as well, my children, my wife.
John Kennedy always inspired us to a sense of what’s called noblesse oblige. Meaning that if you have something and you can share it that’s good for other people, you should do so. I’ve learned over the years that my particular gift is I have an ability to learn things and then transmit that information to other people so then they can have it. What they choose to do with it at that point is up to them.
The word doctor doesn’t mean healer, it means teacher. My mission is to get information out. It’s so incredibly valuable for me not just to get the information out but to teach by doing, by not being in a situation, “Do as I say, not as I do,” to set the example. Am I 100%? No, I’m not. No one is. My wife and I have a thing for eating a gingerbread man. We had to find one. We did and we ate it, and it was wonderful.
I’m happy with where my health is today. It is what it is that I’m at my age, I’m still running and doing things sometimes competitively, at least from challenging myself. Maybe that’s a manifestation of doing the work. My focus over my professional life has been brain health. To think that we can tease apart physical health from brain health is absurd. Brain health follows from keeping your body physically healthy.
[bctt tweet=”The word doctor doesn’t mean healer, it means teacher.”]
Exercise is a powerful offset to risk for Alzheimer’s, for example. It’s one of the reasons I do it. I watched what happened to dad and it’s tough. I had the opportunity to interview the daughter of President Reagan and talk about what she went through and how that played out in her life. Been there, done that. That’s ravaging our elderly. If you’re risked of Alzheimer’s, if you live to be 85, it’s 50/50. You can change that risk by what you do today.
That’s an important message because the message we’re getting is, live your life however you choose, and then we have a pill ultimately. “We’re going to make one. Count on us. We’re going to make a pill that’s going to turn things around.” That’s not reality. I do my best. I’m certainly not perfect. I’m constantly competing with myself to do better and to achieve landmarks in physical health and performance that are benchmarks for me. In this time of social media, writing books, doing all the things, and being on your podcast, it’s all part of that messaging. I see that as something I’m good at. I was asked on a podcast, “What is your definition of greatness?” I said, “It’s identifying what your skillset is and then pursuing it.” That’s what I do.
I was introduced to you with Grain Brain. You start that book out by saying this was a personal undertaking for you to try to understand the mechanism of Alzheimer’s more because of your father. Was that a moment where you departed from a more traditional practice to this broader communication?
Ironically, it was not. You would think that would be the inspiration enough. I had started fifteen years prior. I was into mainstream practice and I had become disenchanted with the notion of treating symptoms and ignoring the underlying disease. Treating the smoke, ignoring the fire. Even back then, there was plenty of literature talking about how lifestyle choices influence your brain’s destiny. I thought, “This is great stuff. Why are we not talking about this?”
I was in a practice with two other neurologists and I started, believe it or not, talking to my patient about the food that they eat and they would have no part of that. It became clear I couldn’t stay in the practice. I went and opened up my own little clinic with two employees. My partner said to me, “Good luck. No one’s going to come to see you if you’re going out the left field with nutrition and all that stuff.” I happen to say that we became busy. It looks like there was an interest in that.
Strangely, when my dad was declining, here I am seeing Alzheimer’s patients all day long and I failed to recognize it in my own father. I remember the exact moment when I finally got it when he was saying things to me that were nonsensical. I said to myself, “He has Alzheimer’s disease. How could I have missed it?” I missed it because I could never imagine my father, a brilliant brain surgeon. I put him on a pedestal and still do. That wouldn’t enter my consciousness that he could have Alzheimer’s disease and when I finally got it, it was a moment because I knew what his destiny would be.
It was interesting because he ended up residing in an assisted care facility that shared a parking lot with my medical practice and my neurology practice. I would see him from 7:00 AM to 8:00, then walk across the parking lot and go in and start seeing Alzheimer’s patients. They’d say to me, “Doc, you don’t know what it’s like to have your parent have this problem,” and I would look out the window.
Oftentimes, I would say, “Matter of fact, I do. My father is in that facility that you can see right there and he’s suffering from this so I do get it.” Though it hurts and it hurts me even now to talk about it, it ultimately had an upside making me more compassionate with them. It helped my understanding and did motivate me, though I had already been involved in this.
Looking at the other factors, lifestyle, etc., pushed me even further to spend more time and learn as much as I could and write a book like Grain Brain that resonated. People got that. They realized suddenly that their brain health and their entire metabolic health well beyond Alzheimer’s were in their hands. It wasn’t something to be offloaded to the next great wonder pill that your doctor may have for you.
I want to get into metabolic health because I feel like a lot of times, people compartmentalize things. They go, “I have diabetes,” or, “I have high blood pressure,” or, “I have Alzheimer’s,” but sometimes it’s the same situation that’s causing all of these problems. They’re just expressing themselves differently in people.
It feels like in Drop Acid, you’re drilling down a little further. I remember this reading in Grain Brain. For example, I already have an artificial knee from years of jumping and I had knee pain. Your body lets you know, “Shoulder, this hurts.” You said, “Your brain can’t let you know it’s in a state of chronic inflammation.” You have this window of time where you’re okay but it’s almost like if you pass over in this inflammation or how long, that’s maybe where there’s a real problem. Do you feel that that’s still the same way when it comes to Alzheimer’s?
Even more so. Early on, when we began talking about that, that was new information. Alzheimer’s the brain on fire. Now, we recognize that people are certainly far more aware of inflammation because of COVID and the so-called cytokine storm that’s been described where these inflammatory chemicals are exploding throughout the body and damaging everything in their wake. Including the heart, the lungs, and the brain. People get that.

Drop Acid – Restorative sleep is a tonic. It’s powerfully effective in keeping you healthy.
There’s also a consideration of the cytokine drizzle that while the levels of these damaging chemicals may not be as pronounced, the fact that they’re acting over a long period of time, nonetheless, is damaging to tissues. The brain is exquisitely sensitive to these inflammatory chemicals and they are upregulated or turned on in the Alzheimer’s brain. We can measure these inflammatory chemicals. They have funny names like tumor necrosis factor alpha, which you can measure in the spinal fluid and demonstrate that it’s elevated and that brain is clearly on fire.
What that causes us to do is to take the step back. What is the relationship between these problems with our metabolism? What is the relationship of inflammation with being overweight or obese, with having elevated blood sugar, being insulin resistant? It’s direct. Higher blood sugar changes our proteins and makes them more inflammatory. It’s a process called glycation. When our proteins bind sugar, it amplifies inflammation.
Body fat is a reservoir that makes these inflammatory chemicals. They come from our body fat. It comes from having leakiness of the gut. Whereby chemicals that should stay in the gut make their way into the systemic circulation and challenge our immune system, turning on the production of these inflammatory chemicals. When they act unabated for a long period of time, the brain can’t defend itself and it begins to suffer. What are the markers? You know when your knee is hurting and you know when other joints in your body are hurting because they turn red, they are painful, and they may swell but you don’t know that in your brain. You know it when you become forgetful, you can’t remember your Wi-Fi passcode or your grandchildren’s names and you begin having these so-called acceptable senior moments. There’s nothing acceptable about them. They are harbingers for a future of brain decline.
How do you measure this? One of the simplest measuring tools that we can to get a sense as to what level of inflammation you have in your body is a sophisticated tool called a tape measure. You put it around your waist and right away you know if you are at risk for increased inflammation. There’s a direct correlation between the size of your belly and the level of these damaging chemicals in your body. It doesn’t take much.
You might have a blood sugar measurement or an average measurement called A1C. Most people are familiar with that. Elevated A1C, even mild elevation, is strongly correlated. In fact, in Grain Brain, you’ll see a nice graph that shows the degree of brain shrinkage over time with increasing A1C, your average blood sugar. That is a metabolic marker. It’s part of your metabolism, what is your blood sugar.
The exciting news is that in the context of our ancestors, this was a survival mechanism. Making more body fat, having a higher blood sugar level, higher blood pressure, higher levels of inflammation allowed us to survive for 99.9% of our time on the planet. These were things that pave the way for our survival. With all the abundance of food and our more sedentary lifestyle, lack of restorative sleep, lack of connection with nature, these issues are going to a place where they’re not coding for survival and how incredible it is that even before COVID, our longevity is being compromised.
The average lifespan in American adults is declining. It’s because we are metabolically in a bad place and getting worse. 1/3 of Americans are obese and in 2030, that’s the distant future, that number is going to be 50% of American adults not just being overweight, but obese. We see that 10% of children between the age of 12 and 19 have hypertension. There’s a lot of work that needs to be done. This is not because our genome suddenly changed. It’s because of this relationship between what our genome is expecting and what we are presenting our genome with in terms of the environment, food, sleep, exercise, etc.
I’ve seen you talk a lot about the conflict between our biology and our modern lifestyles. I feel like this gets talked about a lot and everyone goes, “It’s terrible.” On the telephone and social media, “It’s terrible.” Unless the individual takes control of themselves, then it starts there. I almost feel like businesses, schools, and all these things, we have to figure out how we can put systems in place because I don’t think most people can get there on their own.
Unless you created a tight-knit community and everyone’s rallying behind everybody about meeting to exercise and figuring out what meals they’re preparing, or what have you, it’s a hard undertaking for a lot of individual people. At the top of this, it feeds into a natural impulse more for us like all of these things.
I’m always curious, besides trying to get everybody informed and giving them clear directives like, “These are some things you can do or test,” how we’re going to collectively, the entire group, help pull ourselves out of this. I always believe you have to stay hopeful and it is all hands on deck right now. It is fascinating to watch.
Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar–Your Brain’s Silent Killers
Getting back to your original question to me about the motivation, it’s to level the playing field because people are getting messaging based upon their inputs, social media inputs, television inputs, that live-your-life-however and modern medicine is going to fix your problem. The level playing field is one that says, “It’s all well and good. Medicines are great.”
At the same time, recognize that you got into this mess because you were not eating appropriately. Here’s what you need to do. Here’s the empowering information for you to make better choices. I didn’t think this was going to be the topic of our discussion today but it’s interesting. We wrote about it in our book called Brain Wash. The problem is that this same inflammation that you and I are talking about is bad for the brain, bad for the heart, bad for how our bodies use insulin, etc. This same inflammation takes us away from the better decision-maker part of the brain and locks us into the more primitive amygdala decision-based paradigm whereby we don’t make good decisions.
Inflammation locks us into poor decision-making and takes this prefrontal cortex offline. We make poor decisions and that even includes in our lifestyle choices, the foods we eat. Let me unpack a little bit of what I said. We rely upon this prefrontal cortex, this advanced part of our brain to be the adult in the room, and rein in a top-down control over the more primitive part about, “I want that jelly doughnut. I want it now because I want it. It’s for me. The rest of the world be damned.”
We say using the prefrontal cortex, that more advanced part of the brain, “Jelly doughnuts might raise my blood sugar. I’m going to gain weight.” That connection, that top-down control is threatened by the process of inflammation. Our modern Standard American Diet, SAD, has become the Western diet. It’s pro-inflammatory and that’s the global diet now, highly processed foods.
The global diet is pro-inflammatory. The global diet is taking the prefrontal cortex offline around the world. People are making more decisions about what they want right now for themselves with no consideration of how their actions affect other people, affect the planet, affect the future. It’s quite a concept to embrace this change in global decision-making based upon how the diet of the planet has changed.
60% of it is processed foods, at least in the US, or something like that.
Let me add because it’ll get to where we’re going to go. Of those processed foods, that north of 60% of the foods in the grocery store that carry a barcode have added sweetener. By and large, that is fructose. Fructose becomes uric acid. Uric acid is the alarm signal telling your body, “You’re not going to have food or water. You had better make fat.” It’s hard to resist.
Everybody, yourself included, on the planet has a sweet tooth because it’s a powerful survival mechanism. If it weren’t for the sweet tooth, we wouldn’t have sought out those ripened berries that were at their geek of nutritional value that triggered us to have this system whereby we would make fat and we could survive.
I wonder if they’re going to use technology to figure out how to temper the prefrontal cortex. I almost start to think they’re going to hook everybody up to something that controls it from that top-down.
Gabby, it’s already happening.
I was going to ask you if you’ve heard confirmation about it.
Social media screentime immediately tends to favor your connection to making decisions and acting from the amygdala. What do you think popup ads are designed to do? What do you think all this messaging, the fear-mongering is all about, which then at the end of that event has a call to action? It’s all about activating the amygdala to cause you to respond impulsively. Impulsive activity comes from the amygdala. That’s why we impulse buy. It’s to satisfy that part of our brains and take that prefrontal cortex offline.
Here’s what’s even more worrisome. Those areas of the brain that are light up with pleasure and we seek to a turn on, we can map that now using functional MRI. Functional MRI is being used in what used to be called focus groups to determine what type of advertising is going to light up those parts of the brain best in terms of selling our product. That’s scary business.
I’m saying it is the reverse where maybe somebody comes up with something that people can hook up to get that prefrontal cortex in the driver’s seat.
That’s already there and it’s using one of the various apps for meditation or meditating without an app. There are devices that allow you to enter into a state of consciousness that through biofeedback, lets you stay there, that measure what’s called galvanic skin resistance, a little thing. You can light up your prefrontal cortex.
The more you do that, the more that prefrontal cortex is online, the better is your decision making, the better is this top-down control, bringing the adult back into the room and reining in that 6-year-old. That’s why 6-year-olds don’t drive cars and make adult decisions. You have to be 18 to do this or that, to vote, to buy alcohol, whatever it may be because we know that as we gain years, we gain better decision-making ability. Unfortunately, nowadays, we can leave it at that.
[bctt tweet=”We’ve got to push. It’s not that I want to be outside the box ultimately. I want the box to be bigger. I want the box to be expanded to embrace these forward-thinking ideas.”]
If somebody is 30 years old, an adult but still quite young, besides supporting with lifestyle, food, exercise, relationships, moments of quiet, and being out in nature, when they go to get their checkups, is there something that someone can ask for to say, “I want to check certain things.” Inflammation markers or what have you. A lot of us tend to yield towards, “Somebody in my family had it, so that means I’m destined for it,” versus the relationship of lifestyle. Let’s say they think, “I want to stay on top of it.” You know this. You’re in this business. People are concerned about Alzheimer’s. Are there things that they can request?
It speaks to the notion of being your own health advocate. People, in general, have always been told, “Be a good patient.” What does that mean? It means to go to the doctor, hear what she or he has to say, and leave it at that. They know best. These days, you have access to so much information that you can be your own health advocate. You can wear a continuous glucose monitor and determine what your blood sugar is from moment to moment and make changes in your lifestyle.
Your food choices, for example, and getting enough sleep will have a positive impact on that particular metric. You can wear a ring that gives you a sense of the quality and duration of your sleep and make lifestyle modifications because we know that restorative sleep is a tonic. It’s powerfully effective in keeping you healthy.
We’re seeing a lot of these decisions and actions coming out of the doctor-patient arena and entering the arena of the personal healthcare advocate position. I’m so in favor of it because when you’re constantly informed about the metrics that you talk about, we can then use that information to make changes.
As it relates to uric acid, you can go on Amazon if you must or wherever and buy a uric acid monitor. It’s not expensive. In fact, we sent you one. You can check your own uric acid level at home and know what it is every couple of weeks, know how you’re doing with regard to this incredibly important metabolic marker. I’m all in as it relates to being informed. Frankly, you might ask a doctor, “What about my inflammation markers? Can I reduce my risk of this or that?” Sometimes it’s said that people tend to be down on what they’re not up on. You can’t assume that everybody in healthcare is up to speed on all this important information.
For example, you getting your genome sequenced and then having a sense as to what foods you might do better on, what drugs you should avoid, all the cool things that you can learn about your personal lifestyle choices based upon knowing what your genome looks. Based upon what your gut bacteria look like. That’s incredibly powerful information. We’re right at the nascent stage of learning how we leverage that for specifically what are Gabby’s best choices. Not for anybody else but just for you.
That’s one thing exciting about telemedicine. If you live in a place and you don’t have an access to somebody that you have this confidence in, there are a lot of people out there. Let’s say someone is doing all the right things and lifestyle but they are a stress case. Their waistline is perfect.
What a terrible thing to call somebody.
Sometimes even being diligent creates a weird amount of stress. I see it all the time in performance. You see it all the time, where people hit the mark and they’re weighing their food. They’re almost having a different form of rigidity. Can that impact your brain and your overall health?
No question. It can create stress, create cortisol, and increase inflammation. That’s counterproductive. There are a lot of people who feel like they’re doing everything that they can. They probably know there are a few more things they could do. I generally believe them. There are times when you wonder but patients say, “I’m doing the best I can. I’m going to the gym. I’m watching my carbs and all that.” That’s why this whole uric acid story becomes so empowering because it isn’t the end-all but it is yet another powerful brand new tool in the toolbox. We thought that uric acid was about gout, end of story. The notion that uric acid is playing such a pivotal role in regulating our metabolism is huge.
There was an article written in 2016 by researchers in Turkey and Japan called Uric acid in metabolic syndrome: From an innocent bystander to a central player. Meaning it’s not that it just happens to be elevated in diabetes, hypertension, obesity, and dyslipidemia, but it’s playing a causal role. When we take the steps, we take the quercetin, we take the luteolin, for example, we reduce our consumption of fructose by not drinking fruit juice or sodas. We make sure we exercise, do all the right things, and uric acid levels come down. That missing link that people knew well had to be out there somewhere.
“I’m doing everything I possibly can. I’m not exactly where I want to be with my BMI,” or, “I’m not fitting into my outfit that I want to wear to my high school reunion,” whatever it may be. “I’m trying awful hard but that specific diet doesn’t seem to be working.” This is yet another tool but this is turning out to be a powerful tool. The one I use is called UASure. You can get it anywhere. Buy it on Amazon, buy it online. We should be sending you one anyway. You can text me or email me and let me know what your uric acid is. I’m interested to know.

Drop Acid – You are called as a parent to set these kids up for the best future, health-wise, that you can.
Let’s talk about the numbers. The standard they talk about is 5.5 but you like it lower.
5.5 is what we like. The standard is seven. If you go to your doctor and have a blood test for uric acid and it’s seven, they’re going to tell you that you’re in the normal range. Two points. Number one, that’s the normal range as it relates only to gout because above seven, then that uric acid forms crystals in your joints and is a big deal. The other thing is I’m not about normal range at all, nor are you. We want optimal. We want peak performance. We want what’s best. That’s where we want to get to levels of 5.5 or lower because anything above 5.5 is when we start to increase the risk for things like cardiometabolic disease.
One study that came out in 2009 involved 90,000 people, 42,000 men and 48,000 women, and followed them for eight years. They found that people with higher levels of uric acid had about a 16% increase risk of what is called all-cause mortality, meaning becoming dead for any reason whatsoever. They had a 38% increased risk of dying of cardiovascular disease and a 35% increased risk of dying of a stroke.
What I found interesting was for every point elevation above seven, from 7 to 8, from 8 to 9, there was an 8% to 13% increased risk of all-cause mortality. Higher uric acid, the higher chance you’re going to die not just of heart disease or stroke but of anything. It’s compelling. Japanese literature is way ahead of this. We have an attitude in America. We lead the pack and we know all this stuff, but there’s great research being done around the world.
You get inspired about this topic by listening to Dr. Richard Johnson and Peter Attia. After probably doing a lot a ton of research, you decided to write Drop Acid. In there, 3% of people that have high uric acid have gout or kidney stones. Everybody associates, “That’s a gout issue.” What about this grabbed you and you thought, “This is something to dive into.” What about their conversation? I know Dr. Johnson was a kidney specialist.
Anything that has to do with metabolic health is going to light me up, first of all. Whether it’s continuous glucose monitoring, intermittent fasting, anything that can pull a lever that would give us better metabolic health, I’m in. Because that’s what my whole mission is as relates to the brain and other things, heart disease, cancer, diabetes, all metabolic issues. Maybe it’s because I was running at the time and things get into my depth when I’m listening to them when I’m running.
There was something special about Dr. Richard Johnson. He’s dedicated many years to this exploration of uric acid and metabolic health in animals and then in human interventional trials. I loved his voice. He was so pleasant, sweet, and dedicated. I wasn’t through with the podcast when I finally pass by my own mailbox. Run is finished, time to stop but I kept running. I did the course again because I had to hear the whole podcast, which was an hour and 41 minutes, which is a long run for me.
I got home and listened to it again, and then I did what anyone would do. I called Richard Johnson. I emailed him and got on the phone with him. We began a series of conversations about uric acid. I realized he’s an incredible man doing some incredible work. My job is to report this, to morph this information in a way that people can use it in their lives. I dedicated this book to him because he’s the one. If I were on the Nobel Committee, I would vote that he would win the Nobel Prize for this discovery. I wrote the foreword to his book on the same topic.
Interestingly though, the first book about elevated uric acid related to high blood pressure, dementia, and depression was published in 1894 by Dr. Alexander Haig. This is not new. How we got so fixated on the gout story has to do with the fact that medicines were developed that could lower uric acid. It turns out interestingly, that two things I mentioned, quercetin and luteolin, which are health food store bioflavonoids, work in the same fashion as the pharmaceuticals that lower uric acid. It’s an interesting picture.
The quercetin was at 500.
There are so many reasons to take quercetin. I’ve been taking it for years.
With COVID, it feels like 1 of the bottom 6 that you always hear about. You hear about vitamin C, quercetin, magnesium, and zinc but it’s always showing up even in a protocol for overall health.
For all the good reasons. Let me go ahead and be a little technical here because I know you’ll enjoy it. I would bet that many in your audience have heard about what I’m about to talk about. Our metabolism is governed by two pathways. One of them is called AMPK or AMP kinase. The other is the metabolism of AMP through a different pathway called AMP deaminase.
By and large, we want to keep our AMP kinase side of that switch activated because when we activate AMP kinase, it tells the body, “No need to make fat. No need to store fat. Go ahead and burn it. Be a fat-burning machine. You don’t need to make extra blood sugar.” That’s what we want to do, activate AMP kinase. How do we do that? We do that by exercise, by taking quercetin. That’s what triggered my thought process just now. It’s where the drug metformin works for diabetics so they don’t make more sugar in their bloodstream, in the liver, gluconeogenesis. We want to keep our AMP kinase activated.
There is a time when you might want to activate the other side called AMP deaminase to make a lot of body fat, to store a lot of body fat, to turn on your blood sugar production, and to ratchet down your metabolism. That would be a time if you’re getting ready to enter a cave and hibernate for six months. That’s what happens in bears. They activate the other side of the pathway. They shut it down.
It turns out that uric acid, when it’s increased, activates the hibernation pathway, if you will, telling our bodies, “Make and store fat because winter’s coming,” and takes us away from activating AMP kinase. It takes us away from being a lean, mean, fat-burning machine. As it relates to that, it’s a fascinating story. In the context of our ancestors, AMP deaminase, making fat, storing fat, increasing our blood sugar, is a powerful survival mechanism. We wouldn’t be here today had it not been for the fact that we had that ability and that ability is something we gained about 14 to 17 million years ago when the Earth became cooler and food resources became scarce.
Those of our primate ancestors who made more uric acid survived. It’s why everyone walking the planet right now has this mutation in the genes that make the enzyme called uricase that breaks down the uric acid. We lost that. We don’t break it down. Our uric acid level is 4 to 5 times higher than other mammals, but certainly not those primates that are around today.
It is thought of for a long time as a waste product and now you guys are talking about it being an important marker, you take an individual path on things, so inevitably, someone’s going to push against you.
I hope so.
Drop Acid: The Surprising New Science of Uric Acid―The Key to Losing Weight, Controlling Blood Sugar, and Achieving Extraordinary Health
With other neuroscientists going, “You should go off on your own if you want to talk about eating vegetables and exercising connected to brain health.” Where do you put that for you as a person? How do you navigate when people go, “Come on, what’s the science on this?”
Been there many times in my life gratefully. I wrote my eighth book, Grain Brain, and one professor who is a bit vociferous, when Grain Brain came out, said, “This is nonsense.” Then five years later, he has incorporated Grain Brain into his Alzheimer’s prevention program at an Ivy League medical school. Truthfully, initially, people can be down on what they’re not up on.
That book was written with an extensive review of the science as is Drop Acid. There are more than 400 references that are reviewed in the back of this book that indicates, “This is not that Dr. Perlmutter thinks about this stuff.” Yeah, I think about it but it’s what our research is telling us. If there weren’t pushback, then we’d be status quo. We can’t be status quo.
Ronald Reagan said that status quo is a Latin term for the mess we are in. We’ve got to push. It’s not that I want to be outside the box ultimately. I want the box to be bigger. I want the box to be expanded to embrace these forward-thinking ideas. Could I be wrong? Absolutely. Am I wrong from time to time? You bet I am.
I learned from those mistakes and then move forward. It’s like Thomas Edison and the light bulb. You will learn from what doesn’t work and you’ll learn then from ultimately what does work. Having said that, I have learned over time to welcome the pushback that I will get with Drop Acid. I’ve gotten it for years, but it’s become a comfortable place for me to be.
A lot of people want to do something new or they have an opinion but it gets increasingly more scary. You as a scientist and a doctor, that’s even another level to deal with because people will come at you. It’s different. I appreciate that your work has that built into it. Can we slide over to uric acid and the relationship with your microbiome?
Sure. As you would probably expect, there are some significant interplays then between a uric acid in the microbiome and the microbiome in uric acid as well. Let’s take a step back. We’re talking about the various organisms that live within us and upon us, so not just in the gut but in our mouths, on our skin, throughout our bodies. Even in the brain, there exist microorganisms, though not everybody’s willing to embrace that. We know that to be true and we’ve adopted a relationship with these organisms.
The gut organisms have a huge role to play in inflammation and in managing metabolic health like risk for diabetes, insulin sensitivity, etc. Those correlate with changes in gut bacteria. When the gut bacteria are not up to snuff in terms of their diversity or their numbers, they can’t maintain the lining of the gut. As adequately in the gut, it becomes permeable or what has been colloquially called leaky gut where things in the gut get out into the systemic circulation and can cause that powerful mechanism called inflammation.
The relationship with uric acid is interesting because uric acid elevation favors in the gut and overabundance of pro-inflammatory organisms. Elevated uric acid is associated with increased leakiness or permeability of the gut lining, amplifying inflammation. Interestingly, what is called fecal microbial transplant, which means taking the gut bacteria and fecal contents from a healthy individual and instilling that into the colon of a person who has gout. Those studies show a reduced frequency of gout attacks, likely because of their effects upon uric acid. Everything’s connected.
The gut bacteria, by virtue of this mechanism related to inflammation, influence brain health. Gut bacteria change the expression of our DNA. They’re changing our life code expression. That’s a heady concept to get your arms around. At the end of the day, once you start thinking about this, you’d realize, “I sure as heck take better care of my gut bacteria because they’ve got my future in their hands. Those trillions of bacteria that are in my gut right now are making vitamins. They’re making neurotransmitters, which means they’re affecting my mood from moment to moment. They’re controlling the setpoint of inflammation. They’re controlling whether or not I have an autoimmune condition. They help to determine our outcome should we get an infection like COVID.”
Interestingly though, more germane to our discussion, a study showed that when you go into the hospital with COVID, those people who have high levels of uric acid are associated with an almost threefold increased risk of ending up in the ICU or on a ventilator or dying. They measured uric acid on admission to the hospital. That’s how profound the elevation of uric acid is in terms of the functionality, for example, of your immune system and certainly, it may be through how uric acid relates to metabolic health. We all know that if you go into the hospital to COVID and you’re obese, your risk of a bad outcome is dramatically increased as it is with hypertension, as it is with having type 2 diabetes, metabolic problems for which uric acid is playing a powerful role.
[bctt tweet=”To walk the talk and set the example is probably the most important thing a person can do in healthcare to get messages across. Same thing as a parent.”]
It’s important for people to know that you can have high levels of uric acid and be quite young. In health, there are so many things that are the accumulation of but also this is something that you could be genetically predisposed on top of with your lifestyle where you can have high uric acid. It’s something for people to consider. I appreciate you even talked about uric acid going down, blood pressure going down. There are these direct great measures. As we start to wind down, I do want to hit the alcohol, the beer.
I don’t know how that’s going to sound but anyway, a lot of people do that. They wind down with alcohol. Great point.
I don’t have a moral issue with alcohol. I personally don’t consume alcohol. I grew up on an island in the Caribbean where everyone consumed a ton of it and it looked like a lot of chaos so it was never my thing. In looking at it, of course, people can be moderate about things. One of the things you talked about is that beer, when it comes to uric acid, is not your friend.
That’s right. There are only three sources of uric acid in your body. Fructose, whether you take it in or your body makes fructose, which it does from consuming salt. Alcohol is metabolized the same way as fructose directly into uric acid. A substance called purines, which are the breakdown products of DNA and RNA both from our own tissue breakdown when we exercise aggressively, certainly for somebody like you as an athlete something to think about. Also, purines are high in certain foods like organ meats, etc. The big issue is, of course, fructose.
When we look at alcohol, it turns out that wine in women is associated with lower uric acid levels could be because of the polyphenols bioflavonoids that are involved in lowering uric acid. In men, wine is a bit neutral. Hard alcohol is associated with increased risk but beer is way up there. Both men and women drinking beer, strong association with high uric acid. Why might that be? Because beer contains alcohol but it also contains a lot of purines because it’s made from yeast. Yeast is cellular. It has a lot of DNA and RNA. When you’re drinking beer, you’re hitting the uric acid from 2 of the 3 pathways, the alcohol and the purine pathway.
Interestingly, I mentioned how ahead of us Japan seems to be. They are now marketing no purine beer, recognizing that purine leads to uric acid. If you’re in Japan, and hopefully they’re making their way to America, you can buy beer that does not have purines. Understanding that alcohol and purines amplify this whole process of uric acid and therefore fat production lets us understand that there’s good biochemistry that explains the beer belly. It’s not something that they get because they drink a lot of beer and do not exercise enough. It’s hard to exercise away from a crappy diet. So it is with beer that you’re targeting this survival pathway by two inroads, both alcohol, and purines. There’s good understanding there.
The other thing I’ll mention is that one of the important survival mechanisms that are involved with laying down extra fat is it’s a hedge against dehydration. When we burn fat for energy, we’re making an awful lot of water. For every gram of fat that we burn for energy, we are exhaling carbon dioxide and we’re making free water for our bodies. This notion of storing fat as a survival mechanism is also a survival mechanism in the context of dehydration.
People need to understand that that’s where this is coming from. That’s why these things happen. When we’re looking like we’re dehydrated and our sodium is getting higher because we’re eating a lot of salt, that is telling our bodies that we are dehydrated better, make more fat as a hedge against dehydration. It’s important to think about that. The camel’s hump isn’t filled with water, it’s filled with fat. As that camel is walking across the desert, it metabolizes that fat. It’s a fat-burning machine but that’s giving it free water.
One of the reasons whales are so fat is because that’s where their freshwater comes from. Frankly, we don’t need that. We have access to drinking water so we don’t need to store fat as a reservoir resource for freshwater. The point I’m trying to make is that you can get into this uric acid pathway by making your own fructose. Salt elevation by consuming fat or becoming dehydrated triggers the process by which our own blood sugar, glucose, is converted into fructose. That turns on this whole cascade of uric acid, our survival pathway saying, “Make fat because we need water.” We’ve known for a long time that a high salt diet is associated with obesity and diabetes, but now we know the mechanism and it involves uric acid.
I have never heard that.
You got to think about why does a candle has a hump? That’s the thing you think of when you’re getting ready to fall asleep at night. We’ve pondered this and now it all fits together. It’s exciting information. You have to give it that it’s cool to finally get some understanding of all this physiology and, and what it means in the context of our past, of our ancestors, and how we are today experiencing this mismatch between our evolution and our environment.
I wrote about that when I was 16 in the Miami Herald in 1971, long before you around, Gabby, that’s for sure. I wondered about what do we do with this outdated machinery that isn’t able to genetically or through evolution adapt to this sudden change in our environment that we are now experiencing, unlike anything humans have ever been exposed to.
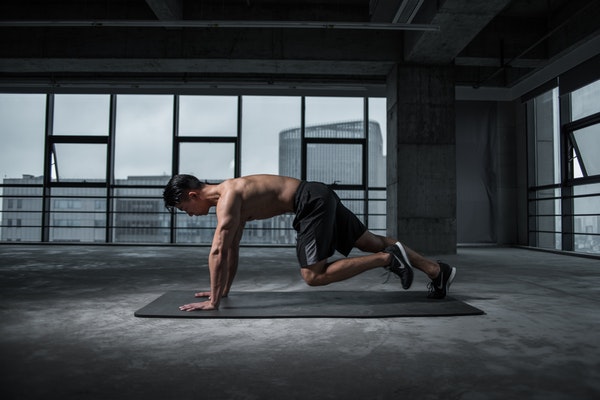
Drop Acid – Brain health follows from keeping your body physically healthy. Exercise is a powerful offset to risk for Alzheimer’s, for example.
That’s the thing, it can feel overwhelming but instead, my hope is that people get this sense of empowerment and that there are people out there that go, “There are tools. It is hard. We’re fighting some biological stuff but we can navigate this little by little.” I know you wouldn’t say to people, “Take these supplements.” We talked about quercetin. This is something that’s confusing and people are always trying to figure out, if there are ones that show up for you that feel important, which ones are those?
First, in the context of uric acid, quercetin, 500 milligrams a day. I can’t say enough about quercetin. Luteolin as well as a bioflavonoid, 100 milligrams per day. DHA tends to offset some of the issues related to fructose consumption, fish oil or there’s a vegetarian form as well, 1,000 milligrams per day. Good old vitamin C, inexpensive, 500 milligrams a day for a number of reasons. We, as humans, don’t make vitamin C. Why that is? We’ll have to do another podcast. The 500 milligrams a day powerfully accentuates our excretion of uric acid.
Finally, one of the biggest issues from fructose consumption is the development of what’s called non-alcoholic fatty liver disease, fat accumulating in the liver. That’s not a good thing for multiple reasons. There is something called chlorella. Any health food store would have it. Chlorella vulgaris is the Latin name. That would be 1,000 milligrams per day.
Those are the key five that I talked about in Drop Acid. There are others that are important. I take supplemental vitamin D every day and supplemental zinc. I take a broad-spectrum probiotic. I take what is called a NAD precursor. The one I take is called nicotinamide riboside. I take about 600 milligrams of that daily.
I also take a supplement that raises something called sulforaphane in my body, either that or I chew broccoli sprouts. Maybe we’ll talk about that another time. I do take a multimineral supplement. I use a lot of what is called prebiotic fiber as a supplement, in addition to eating a lot of prebiotic foods that are nurturing gut bacteria. That’s the reason to take additional prebiotic fiber.
Our ancestors might have gotten as much as 100 grams of fiber a day. Typically, Americans are eating less than twenty grams per day. The prebiotic I take is derived from something called acacia gum. Acacia is that tall tree in Africa that the giraffes are underneath during the noonday sun. It secretes a gum, which is harvested. It doesn’t harm the tree at all. Prebiotic fiber is made from that. As I’m looking at my box mentally, I take a multivitamin as well.
I have three daughters. Two are down the road and they eat well. By the way, one of them in her early teens, there was not a carbohydrate that she didn’t love. I sat back and watched and provided good foods at mealtime but I also let the reins go because I don’t want to make this an issue. I’m going to believe that you’ll go through it and circle around. There are a lot of parents that try to navigate their kids eating.
That’s challenging. Both you and your husband are deeply involved in staying in the best shape that you possibly can and made the various choices, whatever they are, to achieve that, then you want to try to set an example for your children. I know it’s not easy. I have a friend who’s written a cookbook about Alzheimer’s and they seem to have nailed it in terms of how much pressure you exert. If you exert too much pressure, it’ll break, and then you’ve lost all influence.
What we’ve done is we’ve always had dinner at home with our kids, unless, of course, they had some sporting thing that they were involved in, evening soccer, whatever it may be. My wife cooked dinner every night for our children and made them their lunch for school and made them breakfast. Are they visiting their friends? Of course, they did. We all did.
What I’ve noticed that happens with our kids now, since you’ve set an example, is there will come a time when they realize that you are on to something. Generally, what you’re hoping will happen, will happen. They’ll start to see some of their friends that are not as healthy. As it relates to their complexion, they’re going to wonder about the foods that they’re eating. That’s a big thing in the teenage years.
Over the years, people have said, “Dr. Perlmutter, when should we start instituting the Alzheimer’s prevention diet?” What we know now is that we have markers for Alzheimer’s risk that we can see in 30-year-olds that will set the stage for Alzheimer’s 2 and 3 decades into the future. We realized that metabolic issues are profound risk factors for Alzheimer’s, heart disease, diabetes, and cancer. We’re seeing those metabolic issues in people in their 20s, people in their teens, in adolescence.
You are called as a parent to set these kids up for the best future, health-wise, that you can. When does it begin? It begins when your child is in gestation, when you are bearing that developing fetus. What you did then have a huge role to play. How that child is delivered, vaginally or via cesarean section, has a huge role to play in setting up that child’s primordial microbiome. Passing through the vaginal birth canal anoints that newborn with bacteria in his or her mouth, nose, and face that sets the seeds for the development of their entire body microbiome and sets the stage for the level of inflammation. Autoimmunity risk, for example.
When does it begin? It begins early. Getting back to your question, it is a challenge. That gets back to the first question you asked me and that is, do the best you can and set the example. If you want anyone to listen to what you have to say, for me, it’s patients or people involved in my outreach, you have to walk the talk and be transparent. It’s a doctor-patient relationship I’m speaking from right now. You can’t isolate yourself from those individuals with that examining table in middle. We’re all in this together. We’re all at risk together. To walk the talk and set the example is probably the most important thing a person can do in healthcare to get messages across. Same thing as a parent.
I don’t know if you know who Paul Chek is but he used to say, “Your doctor, your trainer should practice as close to the nudist possible so you can see how it’s working for them.” You’re a great example of that. I do want to talk about one thing quickly. We talked about it briefly. When you train hard, it kicks your body’s ass.
It raises your uric acid transiently. Good point. You’re right.
I don’t want to leave that behind because sometimes people will be training and you can almost feel it.
Brain Wash: Detox Your Mind for Clearer Thinking, Deeper Relationships, and Lasting Happiness
There’s no question that you can attune yourself to feel higher levels of inflammation in your body. Your mood will change. Depression is an inflammatory disorder. It brings to my mind this notion of, what are the caveats about checking at home your uric acid level? As I talked about in the book, you shouldn’t train hard the day or two before because you’re going to break down muscle tissue, you’re going to liberate these purines, and they’re going to be metabolized into uric acid.
It’s correct. It’s not an error. It’s going to be elevated. Not that you shouldn’t train hard. You should but be prepared. If you happen to check your uric acid that next day or the day after, it might well be elevated. You should not be surprised if during fasting, if you are a person who likes to fast from time to time, your uric acid level is going to be elevated. Why? Because you’re catabolic. You’re breaking down your body’s tissue to make glucose and you’re using hopefully fat at that point as well. That’s going to kick up your uric acid level transiently.
Your uric acid level will return to baseline within a couple of days after you start eating again and maybe a little bit improved. I would avoid alcohol the night before a uric acid check as well. I’m speaking to this idea of being involved, checking your uric acid, learning what it’s all about, having your doctor draw blood tests or buy a kit and do it at home. This is a powerful tool and it also speaks to the notion of even more reason why when you’re intensely training, especially at a level that you’re not so used to, you want to be thinking about things like vitamin C, especially quercetin. There are a number of brands out there.
I take 1,000 milligrams of quercetin. In the book, I mentioned 500 milligrams. Why? Because that’s what the literature talks about. I take 1,000 a day because even at my age, I push it to a level often that I know based upon what I’m reading on my Apple watch. I’m there. My pulse rate is where I want it to be for an extended period of time. I want to do the best I can to offset even that transient elevation of my uric acid and all the other great things. I’m dialed in on that. You brought up some good points.
I want to bring that up because a lot of times when we’re doing the right things, there are temporary moments where you don’t feel like your best and that’s also for the course.
One step back, two steps forward. Oftentimes, that stress is ultimately good for you. We call it hormesis. It’s good to stress your body. It’s good to stress it with exercise, with hot and cold, being in a sauna, being in cold immersion. As you well know, these are transient stresses that create pathways for regaining health, reducing inflammation, quenching, free radicals, and all the things that your audience certainly knows about.
I feel like if I do those positive ways, I do it less in the negative ways. I’m not picking fights of anyone. Dr. Perlmutter, I appreciate your work and your book is out, Drop Acid. I always encourage people to buy the actual book because it is also a reference and there is so much information. Will you have it on audio?
Audio and eBook as well. I don’t like to travel with them. That’s when an eBook is better. I go through highlighter pens. I’m constantly replacing my highlighter pens. Yellow is my color of choice. I highlight my books, and then what I like to do is go back and read the highlights. I know that you can highlight a PDF. I get that but old habits die hard.
Dr. Perlmutter, can you remind everyone, the book is Drop Acid, all the places that people can find you if they also want to look at your other books, which I would encourage them to do?
My books are all on online retailers. I’m at my website, which is DrPerlmutter.com. That’s where you’ll find links to all the things, Facebook, Twitter, Instagram. I haven’t adopted TikTok yet but who knows? My team is pushing that. It’s quite enough if you ask me. One other thing I will mention, I do have a YouTube channel called The Empowering Neurologist. That’s where I get to interview interesting thought leaders and gain their wisdom.
Subscribe to The Gabby Reece Show
[podcast_subscribe id=”5950″]
Resources mentioned:
- Dr. David Perlmutter
- Grain Brain
- Brain Maker
- Drop Acid
- Dr. Peter Attia
- Brain Wash
- Uric acid in metabolic syndrome: From an innocent bystander to a central player
- UASure
- The Empowering Neurologist
About Dr. David Perlmutter

Dr. Perlmutter is a Board-Certified Neurologist and five-time New York Times bestselling author. He serves on the Board of Directors and is a Fellow of the American College of Nutrition.
Dr. Perlmutter received his M.D. degree from the University of Miami School of Medicine where he was awarded the Leonard G. Rowntree Research Award. He serves as a member of the Editorial Board for the Journal of Alzheimer’s Disease and has published extensively in peer-reviewed scientific journals including Archives of Neurology, Neurosurgery, and The Journal of Applied Nutrition. In addition, he is a frequent lecturer at symposia sponsored by institutions such as the World Bank and IMF, Columbia University, Scripps Institute, New York University, and Harvard University, and serves as an Associate Professor at the University of Miami Miller School of Medicine.