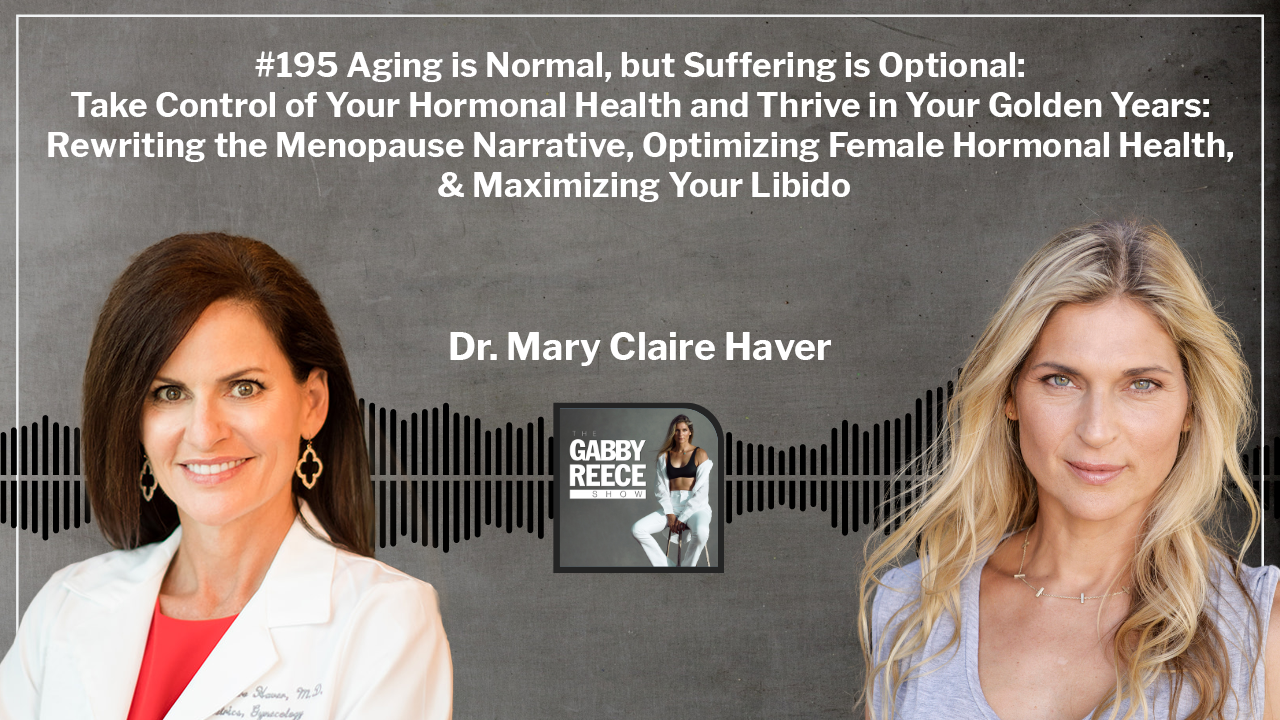
My guest this week is OB/GYN Dr. Mary Claire Haver, the founder of the Galveston diet. Dr. Haver’s mission is to help women improve their hormonal health, regardless of age or stage of life. During our conversation, we dive into the lifestyle practices and supplementation that can support women through menstrual cycles, perimenopause, and menopause. We also discuss the healthiest birth control solutions available. Dr. Haver created the Galveston Diet while navigating her own perimenopause, and it has helped countless women lose weight, maintain their energy levels, and avoid brain fog. Enjoy.
This episode is Part 1 of a two part series on hormonal health. Dr. Haver’s expertise is in women’s hormonal health through perimenopause and menopause. Part 2 is a discussion with Dr. Kyle Gillett more specific to male hormonal health.
Show Buckets:
– Building Your Effective Hormonal Toolkit
– The Female Fasting Formula: How to Reap the Benefits
– A Scientific Breakdown of Women’s Sexual Function
– Taking Charge of Your Hormonal Health: Essential Supplements & Tests
Listen to the episode here:
[podcast_subscribe id=”5950″]
Key Topics:
- The Galveston Diet Genesis [00:04:10]
- Defining Menopause [00:10:53]
- Working Around Menopause [00:15:46]
- Fasting on Women [00:32:31]
- The Menopause Toolkit [00:35:23]
- Food and Supplementation [00:38:07]
- On Birth Control [00:47:09]
- The Connection Between the Gut Microbiome and Diseases [00:50:48]
- Hormone Replacement Therapy [00:55:37]
- Advocating For Yourself for Hormone Therapy [00:58:22]
- Supporting Sexual Health [01:08:15]
- Testosterone in Women [01:10:37]
- Never Too Late to Be Healthy [01:12:18]
- Hormones and Getting Pregnant [01:14:25]
- Sex Health [01:19:01]
- On Alcohol [01:25:20]
- Additional Health Support [01:27:01]
#195 Aging is Normal, but Suffering is Optional: Take Control of Your Hormonal Health and Thrive in Your Golden Years with Dr. Mary Claire Haver: Rewriting the Menopause Narrative, Optimizing Female Hormonal Health & Maximizing Your Libido
Welcome to the Gabby Reece Show where we break down the complex worlds of health, fitness, family, business, and relationships with the world’s leading experts. I’m here to simplify these topics and give you practical takeaways that you can start using today. We all know that living a healthy balanced life isn’t always easy. Let’s try working on managing life a little better and have some fun along the way. After all, life is one big experiment and we’re all doing our best.
—
“If I could go back and tell my 25-year-old self anything, it would be to stop doing aerobics to focus more on muscle building because the muscle you go into this process with is what is most likely going to keep you healthy. Decrease your risk of diabetes and insulin resistance and inflammation. We were focused on thin and not strong. Now, when I’m counseling my patients, I’m like, “We’re working out to be strong, to have a strong heart, to have a strong mind, and to have strong muscles and bones. We’re not working out to be thin, that is a fallacy.”
—
“We live in an obesogenic society and everything around us is trying to make us gain weight and gain fat in places we don’t want or need it. Untangling how difficult this process is important. Most obesity medicine specialists feel that if we can get the lifestyle changes put into place and sustainable for this patient, she may be able to get off the medication and sustain her weight loss.”
—
My guest is Dr. Mary Claire Haver. Dr. Haver is an OBGYN. She has something called The Galveston Diet. What I will say is we are going to talk about all things women and hormones. Simultaneously to this show, I will be releasing, because I never like to leave anyone out when I can, Dr. Kyle Gillette, that is more male-skewed. Having said that, if you have a daughter, a girlfriend, a wife, a sister, or a mother, you might want to pay attention to this because Dr. Haver has a natural knack.
This is not what she intended. She had a practice but then things shifted in her own life. She had lost a brother, created a lot of stress, had gained a bunch of weight because she was moving into her late 40s, and she realized, “None of this is working.” Not only did she figure it out for herself, she even went back to school to understand deeper about nutrition, but she also wanted to figure out how to do it for her patients, what systems are in place, and what programs around lifestyle can we help people whether they’re younger.
Now, she’s specializing in perimenopause, menopause, post-menopause, and maybe even things you want to do to avoid making that harder later. She is good at communicating. I know it’s funny to say, she’s almost become a TikTok sensation if you will. She has incredible programs that involve exercise. There’s hormone replacement. If you have questions about that, we talk all about that.
She has The Galveston Diet. She’s helping women understand the amount of control that they have but it still does come from lifestyle and that you don’t have to suffer through these parts of your life whether it’s your cycles or menopause. There’s much out there that we can do to make it a lot easier. If you’re not interested in all things women and hormones, head over to Dr. Kyle Gillette. Read them both and I hope you enjoy.
—
Dr. Mary Claire Haver, thank you. I wish this is one I could do in person. I always want to do my interviews in person but I was like, “This would be one.” If you ever come to California, I would love to have you on.
Absolutely.
You have The Galveston Diet and book. Where are you?
Physically, I’m in Galveston, Texas. That’s where I live.
You’re trained as an OBGYN and also in culinary medicine, you went back to school for that. Are you surprised that you have a big following online in this communication? I know you had your own experience. You have children. I’m curious if everyone’s like, “This is unusual what you’re doing now.”
I was your bread-and-butter OBGYN physician for twenty years. I also was helping to run a residency program. I was at a big academic institution and I thought I would do that until the day I retired, which would probably be close to death. COVID threw us some curve balls. My own menopause threw me curve balls, my realization of the lack of my own knowledge and education around menopause and menopause care. I was absolutely fine. I can deliver a baby like nobody’s business. I can do a pap smear.
Where I realized was a huge gap in my own education and knowledge was nutrition and menopause. I thought, “I’m curious about the nutrition part because we learned zero in medical school and residency.” Good nutrition was like porn, you know it when you see it. That’s all we got. Going back to school, getting a good background in medical nutrition, and how it applies to medicine, inflammation, and all the things opened my eyes. What began as a conversation about menopause and nutrition exploded into all things menopause.
I would have followers and patients say, “Do you think my frozen shoulder could be related to menopause?” Enough people would ask me that I would go, “Huh.” I’d start looking it up and be shocked by the amount of data around menopause status, perimenopause, menopause, and musculoskeletal issues. It took me down rabbit hole after rabbit hole. It’s where I’m meant to be right now. I did a good job at being a good basic OBGYN but now I’m a menopause specialist and I love it.
It gives you credibility. I will say you have a knack. Your communication, you have such a natural talent for communicating it. Is the frozen shoulder because of a lack of protein and lack of resistance training or is it a hormone?
It’s a little bit of everything. It’s how we’re moving at that stage of our lives. Estrogen, as it turns out, is a powerful anti-inflammatory hormone. There are estrogen receptors in every organ system in our body including the musculoskeletal. When you take that estrogen away combined with the nutrition things we got away with in our 30s, we have endocrine aging, which is what’s happening to women specifically with our ovaries, and chronologic aging as everyone gets older. We lose elasticity and lubrication. That process seems to be accelerated in the menopausal state, the beginning of perimenopause, and we’re seeing this increasing amount of joint dysfunction.
[bctt tweet=”Aging is normal but suffering is not.”]
We live in a way that’s less natural than we used to live. The great thing is we are living longer. I am curious, let’s say 200 or 300 years ago, is there a concept of how women went through menopause differently based on lifestyle? I know that they didn’t have access to certain care that we have now but they certainly didn’t do on a daily basis some of the things that we’re doing now. Was there any information or did you come upon any literature about how it used to be?
From an anthropological point, because of modern nutrition and modern medicine, our reproductive lives are increased is an easier way to say it. We go through puberty earlier than we did generations ago and that’s mostly due to improved nutrition. We are extending our lives because of modern medicine. Don’t shoot me but vaccinations are a huge part of why we live long. We’re not dying of infectious diseases. We’re not succumbing to certain disease states. We have medications. We’re not dying of infections because we have antibiotics, antivirals, etc. The average life expectancy was shortly after when natural menopause hit.
The age of menopause is a little harder to tell. It’s when they could document that a woman stopped childbearing. Back in the day, there was no contraception and it was only nursing a child that would keep your children spaced out long enough to help you survive. Why is there menopause? It’s only us, killer whales, and some species of giraffes that have menopause. Every other mammal seems like they are able to reproduce up until the time of death.
There’s a grandmother hypothesis and it started with whales where the grandmothers have a specific job in the community. They help raise the young ones while the moms go out and hunt. It ensures the survival of the species. At this conference I was at, someone was postulating, “Why would it be an environmental advantage for a woman to go through menopause?” We died shortly after. It was rare that you would have this grandmother that lived a long time.
You and I are about the same age. I’m a little younger. We joke that we weren’t supposed to go through this, we were supposed to be dead. You have to have a sense of humor. I have a large male audience. For covering tracks before we go deep, can we explain exactly what is menopause in simple terms? It’s easy and everyone goes, “She’s crazy,” or, “Open the window, she has hot flashes.” It’s all of that. Maybe we could identify first what it is.
Menopause is the end of the production of estrogen, progesterone, and testosterone from our ovarian tissue, the death of the ovaries. The average age that it happens, at least in North America, is age 51, but 45 to 55 is still normal. Perimenopause is the beginning of that process. You don’t wake up with your ovaries dead. We go through a process called perimenopause where you have this rollercoaster effect of hormone status on a day-to-day, week-to-week, and month-to-month basis until the ovaries peter out at the end.
It’s similar to what you go through in Hashimoto’s Disease where you have this burnout phase and then no production whatsoever. That begins 7 to 10 years before the period stops. We’re looking at a woman, probably a good third of her life, being in this menopausal state. What might that look like to a woman? Eventually, her periods will stop if she still has a uterus. That’s the outside physical hallmark of what’s going on.
Because there are estrogen receptors in every single organ system in our body, nothing gets left behind. We’re biodiverse and everyone’s symptomatic milieu is going to be different. 85% of us will have hot flashes, which is the menopause trope, the woman’s sweating but the big ones are sleep disruption. What has shocked me in my own recent studies are the different medical societies identifying independent risk factors, for example, heart disease, musculoskeletal disease, neurological disease, brain dysfunction, mental health disorders, and genital urinary symptoms outside of just chronologic aging.
Let’s say we took identical twins and one of them lost her ovaries due to cancer or something, some medical reason why she needed to have her ovaries removed at 45, and her twin went through menopause naturally at 55. Even though they’re biologically the same, the 45-year-old will now have a significantly increased risk of heart disease, hypertension, diabetes, stroke, decreased quality of life, and increased visceral fat gain even though they eat the same thing and move the same way. This loss of estrogen production and progesterone and testosterone leads to long-term consequences in our bodies.
I feel the pendulum swinging back. In 2019, you went back to school because you realized how you were feeling trying to fast, diet, and not having the results that you wanted. You started recognizing this gap in nutrition so you went back to school for culinary medicine and you even had to take your boards and do all that again.
What’s interesting is I saw a pendulum in the ‘80s and ‘90s where it was like, “Medicaid or figure uterus out,” sweeping like this. Now, I see the pendulum correcting “real doctors” saying, “Let’s treat the person holistically. Let’s address nutrition.” I feel hopeful because even when you talked about hormone replacement, there was bad voodoo around that. The conversation is moving into an interesting sweet spot with people like you who are blending East and West and taking the whole person into account.
Regardless, even if you’re healthy, I still have my cycle, it feels like it’s sputtering out a bit. Overall, I’ve had a pretty healthy adult life. I didn’t even drink alcohol in my adult life, training, and things like that. I’m probably setting myself up for the best-case scenario. It’s also maybe getting into the relationship of parts of it are inconvenient. You don’t always feel great.
My hope is to get a lot of information out in this conversation but also to remind people it’s like training. I’ve had surgeries before and they want to give you tons of pain meds and I go, “It’s going to hurt.” There’s a part of me that wants to remind people that even if it’s great, you can get weird headaches. It can be a pain in the butt. You can feel more tired and that is maybe a part of it if that makes sense unless we check out and we medicate. That’s also part of the experience too.
I still see patients. I’ve focused now on menopause care. When a woman walks out of my office with a treatment plan, it’s not like, “Here are your hormones, one and done.” We have a conversation about that. We go over the risks and benefits. We make a decision together whether or not this is something she’s interested in and if she’s a good candidate for it. The most important thing I talk to them about is nutrition.
The second most thing I have talked to them is about movement. I have a body scanner in my office so I’m able to measure muscle mass and visceral fat levels. I direct nutrition and exercise recommendations. I’m not a personal trainer. I’m not qualified to develop a program for someone but I’m like, “You need to focus on resistance training,” all women should be.
If I could go back and tell my 25-year-old self anything, it would be to stop doing aerobics and focus more on muscle building because the muscle you go into this process with is what is most likely going to keep you healthy, decrease your risk of diabetes and insulin resistance and inflammation. We were focused on thin and not strong. Now, when I’m counseling my patients, I’m like, “We’re working out to be strong, to have a strong heart, to have a strong mind, and to have strong muscles and bones. We’re not working out to be thin. That is a fallacy.”
How do you get a patient who is a little older and who isn’t familiar? I could see where it’s intimidating. What suggestions do you make, regardless if you’re a trainer or not, to say, “Stick your toe in the water.” Gyms are intimidating for a lot. Imagine you’re 50 and you’re like, “I’m going to bang iron for the first time.”
That’s a great question. If she’s sedentary and doesn’t do anything, we start with walking. I talk to them about walking and then adding in maybe some hand weights while she’s walking or getting the one-pound wristbands, and buying one of the weighted vests to walk with. If you have access to a treadmill, walk on an incline on the treadmill to help keep your legs strong. There are ways to ease into it.
You’re right, you have to meet the patients or your followers where they are and then build from there. It’s understanding that this is the rest of your life. We are going to have to work at this because of a process called sarcopenia, which is the loss of muscle mass with age. If you want to lift that grandbaby in 20 years, if you want to climb that mountain, and if you don’t want to plague your children with your chronic disease and them being worried about you all the time, this is what we need to do to stay healthy.

Dr. Mary Claire Haver – It’s hard to find a practitioner who’s going to give you a holistic plan.
Do you see it where you have women maybe who’ve overtrained and they come in and see you?
My most challenging patients are athletes who have enjoyed a certain level of fitness and they are frustrated when they’re tried and true and training is no longer giving them the cosmetic results that they want. They’re still really healthy, they just have a few more curves but they’re in their mindset. Even though they know the mechanics of it and they know the basics but they’ve always been a certain phenotype and they’re frustrated that menopause has thrown them a curve ball and they can’t exercise their way out of it.
Do you talk to these patients? In my whole life, I’ve trained and I’ve controlled things through movement and probably some form of nutrition. That idea of comparing ourselves to ourselves is an interesting thing. Do you show them, “You’re healthy. Look at your bone density. Your fat-to-body lean muscle mass is great.”
We do blood work. I’m like, “Look at your cholesterol. Look at your homocysteine. Look at your calcium.” They are like, “I want to be 120 pounds again.” I’m like, “You probably will have to make changes that aren’t going to promote your health in order to get to that number on the scale and I’m not going to recommend that.”
Let’s talk about the scale, you launched into that. Maybe we could talk about your own journey because I thought it was not only compelling but probably common. A lot of women probably have experienced what you went through. It’s always maybe also comforting to know that even you who knows had to go on a journey to learn and also that you’ve worked your way to a place that you wanted to be.
Outside of pregnancy and maybe the Freshman 15, I had always enjoyed thinness. I thought I worked for it and it turned out probably not much. A lot of it was genetic. Sadly, I based a lot of my self-worth or my view of myself as a healthy person on what the number on the scale said. I’m cruising along. I was exercising regularly. I thought I was eating healthy. I did have the exercise thing nailed.
I had two things happen at once. I had been on birth control pills to control polycystic ovarian syndrome and I had done well on them and had no problems with them whatsoever. I was 48 or 49 and said, “It’s probably time for me to come off and see where I’m at menopausally.” I talked to my practitioner and we decided, “Let’s get off the pill and recheck some hormone levels and see where you’re at.” Right at that time, my oldest surviving brother got sick. He had been dealing with HIV and Hepatitis for a long time and he was in end-stage liver failure.
We get the call that he is in a coma and he had a stroke. I wasn’t ready. I thought I had more time. I hadn’t said the things or had the closure that I wanted with him. I rushed to his bedside. My sister, who’s a hospice nurse, she and I did the end-of-life care. We got him home and he died surrounded by his family. It was beautiful but I lost my mind for a little bit.
I want to say something because I can tell that you’re a strong person. When you were a young kid, you lost a brother. When you are finding out about your brother, you were in the middle of surgery. It’s also putting into focus what you’re dealing with. You have your own family, you have a practice, you’re doing sensitive, important, and dangerous things with people, and then you have the other parts of life and trying to juggle all of it.
I was in the OR and the phone kept ringing. Finally, I’m like, “Tell the circulating staff to answer the phone.” They’re like, “Hang on. You should hear this.” They put the phone in my ear while I’m operating and they said, “He’s had a stroke He’s in a coma. We don’t know if he’s going to make it.” First of all, I should have never said to put the phone in my ear. My husband used to call me to find the kid’s shoes in the middle of surgery.
As they do
I’m not thinking anything of it. They’re like, “You should hear this.” I’m like, “Okay.” A partner came down and scrubbed me out. We were at the end of the case. It wasn’t as dramatic. We had lost Jeff when I was 9 to Leukemia and Bob had never had children of his own. He had had the same partner for 35 years but he treated my girls like they were his and spoiled them rotten. It’s nothing having a gay uncle who’s fabulous and does drag on the side and likes to play dress up and tea parties and all the things. It was fun. He’ll help you try out for cheerleader. He was fantastic.
His death hit me hard. I had some bereavement leave, did all the funeral stuff, went back, and had to go right back to work. I was a robot doctor getting through my day, my cases, and my patients. At home, I had nothing left for my family. I would go in the pantry and stuff myself with whatever. I would buy those delicious goldfish crackers in the giant package and I would eat and then drink wine till I could go to bed. It’s months of that until the grief started lifting the fog. I was still miserable and not sleeping. I had thought that was all grief.
Finally, I’m like, “When was my last period? I’m menopausal.” Disrupted sleep and horrific hot flashes. Suddenly, my tummy was much bigger. 10 or 15 pounds are a lot for me. This gut came out of nowhere. I could hear my brother’s voice, “You got yourself into this. You got to get yourself out. You can’t blame this on me anymore.”
I went back to the tricks that I used to do after babies or if I’d gained 5 or 10 pounds, workout more and ate less to the point of obsession, to the point where I was severely calorically restricting, due in two days, and only doing cardio. It would work a little bit and then bounce right back on. My husband was leaving for a trip and was going out of town for a few weeks and I said, “When you get back, you’re going to have the wife you deserve.” He looked at me, “Honey, I love you. You look great. I don’t care. You’re obsessed and your girls are watching.”
That’s a big one.
That hit me hard. All the things I had said in lectures and stuff, I wasn’t practicing in real life. Still being Type A, I called up the PhD nutritionist at the university I was employed and was like, “What is going on in menopause? I’m struggling. My patients are struggling.” This was the same thing my patients were all complaining of. It’s embarrassing that I’m hitting the pain point of weight gain because it exploded into much more but that’s what brought me to this discussion, the weight.
It’s an indication. Sometimes, unfortunately, we’re only moved by what’s inconvenient to us. When we look in the mirror, that’s sometimes what we respond to. If I say, “You’re becoming increasingly insulin insensitive,” that may not hit you between the eyes. It’s understandable but it’s also important to separate that out from the scale necessarily. As we move through life, we may not weigh the same at 60 as we did at 20.
It doesn’t mean you’re not healthy, you’re not beautiful, and you’re not worthy.
What is going on also? Simultaneously, it’s going, “Is this a sign?” What did you do?
They sent me down a rabbit hole of nutrition research and lots of stuff about inflammation, quality of nutrition, and how registered dieticians measure the inflammatory index of foods. I was like, “This is amazing but I realized there’s such a gap in my education.” That’s when I started asking them, “Do you think I can get a master’s in nutrition?”
Right at that time, Alpha Omega Alpha, an honor society for medical school, I was a faculty advisor. We brought in a guest speaker and he was from Tulane and he ran the culinary medicine program. I’d never heard of it. I was immediately like, “Sign me up. This is it. This is what I want to do.” It was built for advanced practitioners, physicians, nurse practitioners, Pas, and pharmacists to get a good background in nutrition and then add in the medical part on how you would treat patients.
The labs were in test kitchens where we went and we learned cooking techniques and how to walk through different ways to meet the patients where they are as far as food and their pattern of eating and how we can initiate changes that are doable for the long term. It was the best thing I’ve ever done. In the middle of all that, I’m talking to my patients, I’m coming up with plans, and I’m experimenting with things. My patients are my Guinea pigs and they’re like, “Let’s do this.” They’re all menopausal, pre or post. It grew organically into The Galveston Diet.
[bctt tweet=”The longer your ovaries stay alive, the longer you stay alive and in better shape.”]
Did you bring that home? Were your husband and family all like, “What’s happening?”
They were like, “What are you doing?” I started with fasting and suddenly I wasn’t eating breakfast. They were like, “Huh. My little girls were in middle school and early high school at the time and they want to be with their friends and hang out. They were watching but it wasn’t pathologic, it wasn’t a big deal because I was out of the house early in the morning. They wouldn’t notice if I didn’t eat breakfast or something.
I slowly was making changes. They teased me that I was a little bit of an almond mom for a while. There was a video of a woman, it was pasta night at their house, and she was eating salad and sauce. I’ve done that until my kids sent it to me and I apologized. I was like, “I was going through this learning phase of nutrition and trying to diet. Sorry.”
My girls have the advantage of growing up and this generation. They are curvy and they rock it like nobody’s business. If I had been in that shape, that would’ve been considered too big in the ‘80s. They are embracing it, they love it, they know they’re healthy, they move their bodies, and they eat wonderfully for the most part. It’s a different mindset. I’m happy for them.
I always joke that if the Kardashians did one right thing, it was popularizing curves.
Bringing back curves.
Sometimes people say to me, “This is my genetics.” I’m like, “No, you inherited that lifestyle from your family.” They go, “My family is bigger.” We inherit the lifestyle. Do you have in your office this conversation of almost having to get rid of an old belief system and develop a new belief system? That gets in the way of people saying, “This is how we are in my family. We’re bigger.” The women all drop off a cliff after 50 or whatever it is and get big and things like that. Do you have any ways that you prob them a little bit?
We have conversations around defining health and what that looks like to them. Many of us define health by a number on the scale. I show them, we look at blood work and markers of inflammation. We look at lipids. We look at which are your cholesterol and your triglycerides. We look at their muscle mass. I can’t tell you how many times I get to tell a woman, “You have 80 pounds of muscle. I would trade to get ten of those pounds from you. I’ll give you my cholesterol. I’ll give you my hemoglobin A1C.” They’re powerful people and they’ve been told they’re overweight or obese when they have a lot of muscle. That’s the BMI and your weight can’t measure that for you.
It’s true. I’m not using the word average, let’s say they have an average lifestyle. They’re not uber crazy fit.
Typical Western.
I have friends that have said to me, “I’m eating air and moving and I continue to gain weight.” I know that this is something that you hear and this is something that frustrates many women when they’re going through this because it’s like, “What else can I do?” Maybe we can talk about the different types of fat and people getting their heads around the importance of your muscular-skeletal system.
I will say to people reading, if they want to look at other versions of this, Dr. Gabrielle Lyon talks a lot about dealing almost like another organ and Dr. Stacy Sims. When you talk about fasting in particular, a lot of high-performance women perform better fed. I like to try to be as consistent as possible when we’re administering. With fasting, is it also getting control and pulling in the reigns a little bit? What are we seeing that fasting then does for women going through this?
What interested me in fasting was not weight loss. It’s not a great way to lose weight. You can eat terrible things in your window that also undo any inflammatory benefits. I approached it because of some of the data around neuroinflammation and Alzheimer’s and dementia and lowering insulin levels, fasting glucose levels, and fasting insulin levels.
I was astounded. I thought it was a fad. I’m like, “Why would you not eat breakfast? It’s the most important meal of the day.” Whichever your fasting window is, why would we have to limit or restrict how we eat? There’s good data even in women in menopause showing some anti-inflammatory benefits and lower blood markers of inflammation. This is in average women and not high-performance athletes, which is a whole different way. You must feed your body more. The muscles are just going to chew everything up.
For most women who exercise less than four hours a week, fasting works pretty well for them. It is not for everyone. It could trigger an eating disorder or hypoglycemia. I always tell people to ease into it and give themselves six weeks if they’re going to shoot for the 16/8, which is what we preach. I have lots of students who are doing 12/12 and doing beautifully on it. It seems that the medical benefits hit at about hour twelve. If you’re tagging on your food-free window with sleep, it’s not that long.
I love that. I do appreciate you making a suggestion about getting people to build out fifteen-minute windows. Start someplace and then add fifteen minutes.
Do that for 4 or 5 days and then add another 15. See how you feel. Do your workouts. How are you feeling? Listen to your body.
That’s another important thing because we’re going to talk about the things that you’re seeing on average but people trying to stay tuned in to how they’re feeling. A lot of people say, “Tell me what to do.” They’re not checking in. I’m always saying that whatever level of fitness or emotionality or whatever, we can make all the best plans in the world but we still need to understand eating a certain way. Did we get a good night’s sleep or what have you?
I always want to remind people that one size doesn’t fit all. You talk about inflammation as being something and insulin sensitivity is something that we need to stay focused on. She comes in to see you and she’s like, “I’m getting my butt kicked by this process.” Is it blood work? Is it like, “First, we’re going to look at lifestyle.” What’s your approach?
I’m a little bit unique and I have an hour with each patient. I have time with each new patient and then 30 minutes for a follow-up. Also, not accepting insurance gives me that luxury.The blood work is included in their visit. I do everything, I’m checking nutritional markers, inflammation markers, and some hormone markers. In menopause, a lot of conditions can have overlapping symptoms. You think that it’s menopause but maybe it’s hypothyroidism or maybe it’s both.
Some autoimmune diseases can often present similarly to what a menopausal woman would be going through. I have diagnosed lupus twice in the year and a half that I’ve been in the clinic. I’m doing blood work to make sure I’m not missing something outside of menopause. We launch into lifestyle discussions, nutrition, movement, stress reduction, and sleep. It’s all part of what I call the menopause toolkit. Everything works synergistically together to get you to your best health.
In the brass tax on lifestyle, in movement, what are your most baseline suggestions for women?
For resistance training, at least twice a week, you should be hitting all the major muscle groups. I don’t give them time limitations. Whatever it takes, you should plan on at least 30 or 45 minutes per session if you’re going to try to hit all of your body parts. I suggest some of the more popular online programs that I find to be pretty consistent, safe, and reasonably priced.
Fortunately enough, through the years, we’ve accumulated a ton of exercise equipment. We have treadmills and bikes, we have everything. I wish they got used as much as they should. My husband and I gift each other more exercise equipment. Most of our travel is centered around hiking trips and things. That’s how we’ve chosen to find joy and move our bodies at the same time.
Sometimes people think they’re doing a lot of the right things and it’s almost mind-blowing what they’re still consuming and they’re trying to pay attention. I have found that a lot of people in your type of practice say, “We’re not going to add more things. We’re going to try to take out the things that aren’t supporting you.” What’s the conversation around food and how do people approach that?

Dr. Mary Claire Haver – Call in the troops, get your friends, and get that community. Don’t think that you can do this on your own because you need good nutrition, you need support, and your body’s healing.
If someone comes in and they are sarcopenic, they’ve got low muscle mass, and they’re below the 90th percentile, I’m worried that they are going to be super high risk for osteoporotic fracture or being functionally deficient. We have a big conversation around protein intake and a lot of them are shocked at how much protein they need.
If you have low muscle mass and you’re trying to get to normal muscle mass, the rule is about a gram per pound of what you want to weigh. For me, that’s about 120 grams of protein a day. In the Western diet, most women eat almost no protein at breakfast. They’re doing oatmeal or cereal or something and the only protein they have is oats or something. At lunch, they might have a little bit of protein with their salad.
At dinner, they’re saving their protein for that big piece of chicken or that big steak or something. One of the conversations I have is it’s going to be a lot easier if you are working in at least 10 grams of protein with each snack and 20 to 30 with each meal. They’re like, “What?” We walk through what that would look like. If she’s coming in and she has elevated visceral fat, we go through all the health risks associated with that.
If I lock them in a cage and starve them, of course, they would lose visceral fat but they’d also lose everything else, their minds. It’s making sure she’s getting enough fiber. Women aren’t tracking their fiber. They have no idea how much they’re getting. The minimum for a woman is 25 grams a day and I push to 35 personally.
We talk about magnesium and how important that is and trying to get that through nutrition. Supplements are meant to supplement a healthy diet. If you can’t fit them all in one of those little pill boxes, your daily supplements, that’s Dr. Haver’s rule of thumb. There’s no science behind that. Supplements are when you have an allergy and intolerance. The cost is keeping you from being able to get what you need. You should strive to get what you need from whole foods.
There are many different types of magnesium it throws people. Is that for sleeping or going to the bathroom or relaxing? Which one is that for?
All of the above. It depends on which kind.
For fun, can we break down the few types of magnesium and what they do? People are becoming more informed but they’re like, “Which magnesium would help me sleep better?”
There’s bioavailability when we talk about anything we eat nutritionally or any chemical substance we’re trying to use for health, which means, how much of it that we put in our stomach gets into our bloodstream? Different types of magnesium have different levels of bioavailability. The ones that don’t go into our bloodstream and stay in the gut can induce bowel movements. We use mag citrate or mag oxide to help clean the bowels for a colonoscopy. Anybody over 50 out there, hopefully, you’ve had yours. That’s not a fun process but medically necessary. That’s magnesium.
Milk of Magnesia was used for inducing bowel movements. Where is the magnesium glycinate or taurate? Those have great bioavailability. They’re great for raising your blood levels. The one that I tend to recommend the most is to get to the brain. For sleep, for ADHD, and for SSRI, resistant depression, magnesium L-threonate seems to be one of the better ones that cross the blood-brain barrier and that’s what I take.
I do too. I’m not a great sleeper and I never have been. It’s always the dance around. When it comes to supplementing D, we have to have to. I agree with you. If we can get it from food, there is nothing better. If you said, “Let’s cover the basics. These supplements are pretty hard to get in our food.” It’s d and what other ones do you like?
D and Omega-3 fatty acids. There are vegetarian and vegan forms but it’s ALA, which has to be converted to DHA and EPA in the blood so it’s not as efficient. You have to eat a lot more. If you’re a vegan or vegetarian, you should consider supplementing. Nordic Naturals is one that’s algae-based. The fish eat the algae and that’s where the fish get their Omegas from. The bigger fish eats smaller fish and the cycle continues. It all comes from the algae and you can get it from there but it’s a lot more expensive than doing a fish oil supplement.
I’d love to know how you feel about it. Going back to younger women, that’s also supportive to them. I’d love to hear your thoughts on it for their menstrual cycles and things. The Omegas are supportive of the health of the cycle as well.
The Omegas are made up in all of our cell membranes and they have a lot of brain activity. Our menstrual cycles begin in the brain at the level of the pituitary hypothalamus. Whatever we can do to keep that brainstem healthy and functioning, absolutely. Omega-3s in children with ADHD have been shown to be almost as effective as some neurological medications.
That’s what I love about that. You have two daughters. You’ve gone through teenagers and you yourself have been a young adult. I have three daughters. I would love to talk about hormones themselves, estrogen, testosterone, and progesterone. We talked about the Omegas. My girls willingly take that stuff. I say, “If you like it, it’s there.” It’s being an example.
You’re doing a different part of your practice. When you have a younger person and their hormones are finding their way, is there anything else that is supportive besides nutrition and trying to get to bed? Even though, at that age, they naturally stay up later. Is there anything that you did even with your own girls that maybe is supportive of them? That can be a challenging time.
My kids are supercritical. My oldest is a nutrition science major and she’s graduating and starting medical school. She’s verbal about everything that comes out of my mouth and what I might say and not say. She is a big fan of evidence and not cherry-picking evidence to fit whatever your hypothesis is and looking at all the evidence. She’s a big fan of Omega-3 fatty acids. She’s a big fan of vitamin D at almost every age. She’s a big fan of trying to get what you can get through nutrition.
The rule of thumb I advise followers and patients is to track what they’re eating for a week. Eat your normal diet and see where you’re falling low on with the recommended daily amounts. Are you getting enough calcium? Try to use food. Is it easy enough to add in a handful of pumpkin seeds for mag or a little extra serving of dairy for calcium if you can tolerate it to hit those levels? Is that something you should be supplementing? You can do that with kids as well.
My husband is always trying everything in food. He found out that everyone was taking much quercetin and he is like, “Capers.” I’m like, “Here we go. We’re going to be eating how many capers.” Birth control is a tough one. You were taking it for something to manage something else. In a perfect world, if someone is not prepared or is done having children or isn’t there, and let’s say they didn’t have any extra unusual conditions, what do you feel? Birth control is tough on you. What do you think would be maybe the best way to start if someone could tolerate it?
Intrauterine device, IUD. It’s non-hormonal. There are a few different types. The ones that have progesterone in them, it’s a low level of progesterone and it’s locally acting. If you have heavy periods and cramps, a progesterone-containing IUD is a fabulous option. You don’t have to have had a baby. You can put it into someone on the younger end of the spectrum safely if you know what you’re doing. One of the problems that we’re seeing in a conversation I’ve gotten involved in is gynecologic pain and treatment of pain for gynecologic procedures is variable as to what your provider is going to offer you.
[bctt tweet=”You know what’s sad? Probably 10% of women will never orgasm in their life.”]
I was doing paracervical blocks. I’m on oral medication. I was doing everything I could outside of sedating someone for these procedures because they can be traumatic, especially with someone with a history of trauma there anyway. I want someone to have good and adequate contraception or cycle control or whatever the goal is for her medically. For me, IUD is the best option cuz it’s not suppressing her ovulation. She still has normal estrogen function. We’re not worried about bone density loss. That’s usually one of my tops.
Do you address anything with the microbiome connected to hormone health? It’s complicated dealing with hormones.
It is a thing. I’m writing a new book, and the contract is signed and I’ve got the collaborator, on the medical ends of menopause. One of the chapters is on the microbiome and what happens in menopause. Our gut flora and urinary flora are closely tied. The two outlets are right next to each other and they share quite a bit of the same bacteria. We see lactobacillus, which should be the predominant bacteria in the vagina. The vagina is not sterile. In our reproductive years, when our estrogen levels are high, lactobacillus should be number one. Whenever we lose lactobacillus, we can have bacterial vaginosis overgrowth.
A lot of us have dealt with BV over the years or yeast overgrowths. How many times for any of your readers taken an antibiotic for whatever and then ended up with a yeast infection? We killed off the good bacteria and the yeast didn’t have anything holding them back. You end up in a vicious cycle there. In the gut, it turns out that estrogen affects our gut as well and our gut microbiome becomes more like that of a man. At the same time, our risk of heart disease and our health disease risk goes up to a man’s and they’re now thinking it’s more closely tied to the gut microbiome than ever.
In the last five years, it’s mental health, and everything is tied back to the gut, serotonin, and all these things. How do you peel that onion? You have a patient and they’re like, “You want me to eat this much protein.”
Probiotics and fiber. It’s thinking of things in a different way. Fortunately, in my practice, most people have seen me on social media. They’re coming with some level of knowledge. They know what they’re in for when they’re coming into my office. I have a questionnaire they fill out, “Do you understand that Dr. Haver is going to make nutrition recommendations? Are you okay with this?” A lot of them want one of the quick weight loss medications and they want speed. I’m like, “No, that’s not what we do here.” They’re thinking it’s a quick weight loss clinic and it’s not.
What’s that weight loss drug that everyone’s taking?
They’re called the incretins and it’s a class of medications that were originally developed to treat type 2 diabetes, which they do well. One of the things that they’ve noticed in the last couple of years is that they are seeing weight loss with it. Peter Attia talks about this extensively and I like the way he puts it. It’s reaching the number on the scale rather than looking at other measures of health.
What he’s finding in his clinic and what I’m seeing in mine because I have a muscle measurement tool there is we’re losing quite a bit of muscle mass if you’re not careful monitoring protein intake and making sure they’re doing resistance training. It’s a tool to help in someone’s weight loss journey. It should not be the only thing you’re doing. What’s alarming to those of us in this space is that everyone is prescribing it and you’re getting it online without proper follow up and it’s weight loss at any cost. That’s never going to be the right way to go.
For every pound that they’re losing, it’s almost two pounds of muscle. It’s something pretty radical like that.
Half. With extreme caloric restriction, without getting enough protein, and without lifting heavy things over and over, you are going to lose muscle mass. For every pound, half of that is half a pound of muscle.
Because many people are now looking into it and taking it, what is it about it that jumpstarts the weight loss that if you did adjust the lifestyle, you could keep it off? Do you think that is possible?
The obesity specialists do think it’s possible but you have to do all of the lifestyle changes that are sustainable for the long-term to keep it off and be able to get off the medication. What happens in real life though is that’s difficult for a lot of people and they’re excited to get to that number on the scale. As a society, they’ve been driven by this number and that being the only representative of their health.
Doctors do it too and I was one of them. This was willpower. This was you being lazy. Without how complex the factor of someone who’s dealt with obesity and everything that feeds into it. We live in an obesogenic society and everything around us is trying to make us gain fat in places we don’t want or need it. Untangling how difficult this process is is important. Most obesity medicine specialists feel that if we can get the lifestyle changes put into place and sustainable for this patient, she may be able to get off the medication and sustain her weight loss.
It’s an interesting dilemma. For a little bit, I was raised by somebody who was battling her weight since very young. She had childhood trauma coupled with then more of a sedentary life and things like that. In her maybe late 30s or early 30s, this is when aerobics was around, in the ‘80s, it trashed her knees. She lost 100 pounds and then gained 100 pounds back. Was that harder in a different way?
What we’re finding in the rebound weight gain in people who lose that much muscle is everything they gain back is fat.
I only bring that up not as a warning but to remind people that it might be a boost. We live in a time where everyone’s hacking everything. I don’t think that works in the long run. Can we slide over to hormone replacement? I appreciate it because there’s always been like, “If you’ve had cancer in your family…” There’s all this weird voodoo around it.
Most of that voodoo comes from one study, it was the Women’s Health Initiative. The preliminary results were released in my fourth year of residency. It rocked the world. About 85% of women were taken off or self-took themselves off of hormone replacement therapy. Even though that study has been walked back, retracted, and basically debunked most of it, that whole generation of physicians in multiple specialties has worn people away even though we have a plethora of data on the health and safety of hormone replacement in menopause for the vast majority of women being safe.
You’ll hear people talk about bioidentical or synthetic. For people, it’s confusing.
That’s a great question. Let me give you a primer. Bioidentical simply means chemically similar or identical to what your body made. What began as a simple way to explain different forms of estrogen that you can put in your body has become a marketing term and it’s been grossly overblown. Other forms of estrogen have been demonized for no other reason than to sell you a certain thing.
What your ovaries make is estradiol and that is what I give to patients. You can get good, high-quality, efficacious, and safe estradiol from CVS with a prescription for about $25 a month. You don’t have to do pellets, you don’t have to do creams or concoctions. We have great bioidentical efficacious safe hormone therapy that is reasonable and affordable. If you and your practitioner decide that you want to do a pellet or a cream or whatever and if you’re not offered all of the options, I walk through all of the options with my patients, the pros, the cons, the risks, and the benefits of each.
She and I decide what’s best for her and what’s in her budget. In no way am I steering her towards one certain thing, especially one that’s going to personally enrich me through a procedure. That is where I see there are a lot of ethical lines being crossed with patients who are being told, “You must do this. This is the only thing we offer.” Absolutely not, that should never be the case.
Is she getting a new physician? It’s hard for patients to push back.
On my website, I have a blog all about how to advocate for yourself for hormone therapy at your doctor’s office. I have medical journal articles you can print out and hand to your doctor. That has worked, patients have told me. I’ve been in contact with a few of these companies. There are 3 or 4 online companies that saw a pain point that recognized that women are struggling to find healthcare practitioners who are willing to open the discussion with hormone therapy.
You may decide you don’t want it. Your body, your choice. I fully support that. If you decide, “Not for me. I want to white knuckle through this, do the nutrition exercise, and do everything else.” Fine, at least you deserve the conversation. Finding a doctor who will even open that conversation is hard. Where do you turn? I’m like, “Call ahead. Talk to the nurse in charge. Make sure that this doctor will even have a conversation with you.”

Dr. Mary Claire Haver – Everything around us is trying to make us gain weight and gain fat in places we don’t want or need it.
If you can’t find anyone, there are several online companies that are put in this world to discuss hormone therapy with you and act as your advocate. I’m not associated with any of them. I have a list of them on my website where we independently reviewed each one and talked about costs and how they make their money.
There’s one called Midi Health. They do take insurance and they’re probably in 8 or 10 states now with plans to be open in all 50. if insurance is your best option, that’s a good one to try. Evernow is another one and My Alloy. They don’t take insurance but it’s reasonable, $10, $20, or $30 a month for a subscription, and they mail you your hormone therapy that way.
What do you do? Get your blood panels done, they take a look, and then they discuss your options.
This is another fallacy. You don’t need a blood panel to determine if you’re menopausal. If you’re over the age of 45 and you have not had a period for one year, you are menopausal. We don’t need a blood test. Your levels are going to be zero. We know it.
What’s considered post-menopause? Is it from the time you start your period?
Menopause is one day in your life. Your menopause day is one year after your last menstrual period if you have periods. If I have someone who’s had a hysterectomy and she’s like, ”I don’t know.” I’ll do the blood work to confirm it, of course. If she’s like, “My last period was three years ago. I’m having hot flashes. My hip hurts. I’m having headaches.” I’m good. I know enough to not have to send an expensive blood test.
Perimenopause is different. We have this dramatic fluctuation. As anybody who’s been through it, it can rock and roll your system. You feel great one day, you’re crazy the next day, you don’t sleep the next day, and you’re sweating the next day. Hormone levels fluctuate. A one-time blood test, I can check it but it’s rarely diagnostic. Perimenopause can be diagnosed by talking to the patient, listening to the patient, and believing the patient. I’ll do blood work to make sure I’m not missing hypothyroidism or autoimmune disease depending on her symptoms. I’m not checking hormones. I’ll go ahead and start a treatment discussion.
Between estrogen, progesterone, and testosterone, what is each one? Someone used to say, “Progesterone is feel-good and let it roll hormone.” People go, “Why is a woman a little more agro towards her cycle?” The progesterone drops and whatever hormone is lower than usual. Alisa Vitti had a great line where she said, “Keep a journal. For three months in a row, if that same feeling about that employee or partner keeps showing up, that’s how you feel after three months.” What are you prescribing depending on what she’s going through?
If she still has a uterus, we are giving it to protect the lining of the uterus, endometrium, from developing hyperplasia or cancer. When we prescribe hormone therapy in the form of estrogen, we always have to buddy it with progesterone. You don’t give her hyperplasia or malignancy. There are a few patients who are still struggling with sleep and are still having some issues or anxiety. Especially at night if they have racing thoughts, progesterone can be helpful there.
When people have had a hysterectomy or have that progesterone IUD in place, I will sometimes add a little progesterone at night to see if I symptomatically can get them to feel better. It’s not done routinely in women with a hysterectomy. Testosterone is a little different. The only thing that has been medically shown through studies that testosterone can be helpful with is what we call hypoactive sexual desire disorder or what lay people would call libido.
A woman’s sexual function is complicated and there are five buckets of why a woman can be unhappy about her sex life. First of all, she has to be unhappy and not her partner. If you have a mismatch of desires, that is not her fault. We have relationship disorders. If you’re not feeling loved or supported by your partner, nobody wants to do it, I can’t fix that with medication. There is arousal disorder, desire disorder, orgasmic disorder, and pain. If you’re having pain and a lot of menopausal women from vaginal atrophy have pain, we must fix the pain. Usually, if you had a good libido before, it will come back if it doesn’t hurt.
Desire is what happens in the brain. It is that initial, “That seems interesting. I’d like to do that.” Arousal disorder is the physiologic response to a stimulus. The vagina elongates, more blood gets pumped in there, the clitoris gets enlarged, and all the physical things that happen. If that’s not firing, that’s usually a circulation disorder or a nerve conduction disorder that’s treated in a specialist clinic’s office. Do you know what’s sad? Probably 10% of women will never ever orgasm in their life.
Is that emotional and then they never had a partner?
We don’t know. No one will study it and no one cares. If that happened to a man, it would be the end of the world. More money that was spent on the arms race would be spent on fixing that for a man. It’s complicated. We’re not sure. Lots more study needs to be done. There is primary and secondary anorgasmia.
The secondary means you used to do it and now you can’t. There are specialists but they’re very few, they’re overbooked, they’re hard to get into, they don’t have a lot of time, and these are complicated issues to see why this is happening. Is it a nerve conduction disorder? A lot has to happen between this part of your body and this part of your body to have an orgasm and that anybody can do it is amazing. Is she not getting the right stimulation? There are a lot of fallacies around. Every time I see a sex scene in the movies or on TV, I’m like, “This doesn’t happen. This is not a thing. No woman does this.”
It’s true. My husband always jokes, “Is the moon in the right place? Are we good? Are we ready?”
“Is the moon in retrograde?”
I’m like, “It’s not that complicated.” He’s like, “Huh.” That’s the line when they tell the young men, “Easy to please many women once. Try pleasing the same woman many times.” Are you serious though? That many women? I didn’t know about that statistic.
They don’t talk about it. The ones who come to my office who admit it are fine with it. They’re like, “I don’t know what I don’t know. It’s pleasurable. I make my partner happy. No, I’ve never had an orgasm.” It makes me sad for them.
It’s one of the most beautiful things in life, it’s nature’s gift. You’ve been in a long relationship. This is like a philosophical question. This would be true of any person. I feel like when you can be in overall, no relationship is perfect, nurturing, accepting, loving, sexual, growing, and thriving relationship. I feel like it supports that overall health. I’ve met some women in their 80s and I have a friend in particular and she has a look in her eye and I’m like, “She had a lot of love. She’s been well-loved.”
I don’t mean that you can only get it from a partner. Of course, you can get it from your family and your kids. It feels like something worse saying that you would like to try to have. Even to speak up with your partner and be like, “I’m not feeling appreciated,” or, “I’m not feeling loved.” When I think about health, that is a supportive component if you find someone that can support you physically and even your sexual health.
[bctt tweet=”I worked with a therapist for a while and this is probably the best thing I’ve ever done.”]
Where I’m seeing the crossroads for a lot of women who have made it past the divorce state, they’re like, “I’m in. I’m sticking here. We’re going to die together.” It’s that empty nesting. You’ve devoted your whole life to schedules and kids and your schedule and his schedule and everybody’s schedule. All of a sudden, there’s this huge gap. I empty-nested for the first time. My husband was working overseas quite a bit so he’s gone about six months a year. At first, I was dancing through the house by myself, “This is amazing,” me and the dog.
After about a week, I was like, “I don’t like it.” We have had to have multiple conversations about redefining who we are as a couple outside of taking care of children and in every aspect of our relationship, from sexual to household, daily stuff, and division of labor. Plus, all the stuff on social media is making me cognizant. My kids talk about it all the time. They had two working parents and I would leave him with children when I had to go work at the hospital for shifts. I’d be like, “Keep them alive. Bye.” He would bring them to the hospital in dirty clothes and their hair is a mess but they were alive.
That’s great.
He had to do it. He had no choice. His dad never changed a diaper. Seeing that empty nesting, at this age, a lot of us are and how that redefines our relationship.
I always joke that, in a way, when you have kids in the house, you have to consciously have a sex life. When they’re little, it’s like, “They’re sleeping,” or, “They’re at a friend’s house.” In a way, when they’re gone, you have to almost create a new relationship that is about who you are today. It’s an interesting dance. How do you feel about testosterone? I hear a lot from performance people, “Unless you’re having kids, testosterone is also important for women.” Men love testosterone, they want to talk about it, they want to know about it, and they want to know about their numbers. It’s also important for women.
There’s no FDA-approved option for women so that is one I have to compound. I usually do a local compounding pharmacy and we do a cream. We adjust her dose based on her symptoms. Because the sexual response is complicated, probably about a third are not going to see a response. What I’m prescribing it for off-label are those patients with low muscle mass. I am worried about them.
We’re not talking about increasing performance. I want them to get some meat on their bones so that they don’t fall and break in twenty years. Testosterone supplementation with protein intake and with resistance training, those three can be important tools to help her reach that goal. I’m not using it for anything else. I don’t see enough studies for me to clearly say it’s going to make you think better and some of the stuff that people are claiming.
It’s clear, teenagers, 20s, 30s, and 40s, what we’re eating, let’s move enough, let’s lift some weights, let’s get our heart rate going a few times a week, and let’s do some cardio but let’s not get obsessed with it. These are all things that would also make this process a lot easier. Someone is reading and they go, “That’s all great for you guys but I’m already in the pocket. I wasn’t raised to be an athlete. I’m working on my food.” Have you had patients, whether they’re in their 50s, 60s, or even older, can they adapt? Can they shift and impact themselves positively?
Absolutely. I have seen it because I can measure these things, measure their cholesterol, measure their A1C, and measure their muscle mass. I have great indicators of health that I can utilize at any age. I’ve had 60s and 70s. Most of my patients were in their 40s and 50s, “I know I’ve got twenty more years.” I want them to be the best that they can be, “What can I do?” I meet them where they’re at and we start making changes.
I had one patient come in who was coming in three months for her follow-up and she walks in and throws herself down in the chair and says, “I’m mad.” I go, “What’s going on?” She says, “I can’t believe I let myself be miserable for long. Now I feel good. I let myself suffer because I didn’t listen to my body. I listened to what the doctor told me and that I had to suck it up.”
The problem is that many of the physicians are like, “Welcome to this time in your life. There’s nothing we can do. I don’t believe in treating menopause.” Physicians aren’t trained in nutrition, they aren’t trained in exercise outside of having a degree in it. Not the ones outside of sports and rehab medicine. It’s hard to find a practitioner who’s going to give you a holistic plan.
I want to drive that home because people think, “That’s not going to be for me. I missed the boat on that.”
It’s never too late to be healthy.
They could be in their 40s. People throw in the towel and go, “I’m this age now.” I know you’re not maybe working with women this age but let’s say people have had children and they’re dealing with hormones because that’s such an interesting and intensive process for the body. Maybe they’re not getting back to some level of homeostasis. What would you say or suggest for them? I know a lot of people are navigating that, especially if they had to take any hormones to get pregnant.
I went to a menopause symposium and they were likening the postpartum period to menopause. They’re similar on a biochemical basis. There’s an advantage to having disrupted sleep because you can hear the baby better. There are some advantages to it. You don’t have to suffer. What I was telling my patients who were getting ready to have a baby is you’ve got to have resources in place. Don’t expect to go home and be able to do this on your own, especially if your partner has to go right back to work.
Back in the cave days, you had a village helping you take care of the baby. Call in the troops. I never had a great relationship with my mother. She was the best baby nurse in the world. I fell in love with my mother when I had children because she came in, she has eight kids of her own, and she was a boss. She was putting me on a schedule. She was taking that baby in the night. I was like, “How would I do this without her?” She was cooking healthy and delicious meals. I had time to shower. For six weeks, she hung in there with me and she brought me to her house when Chris had to travel. That is how it should be.
Call in the troops, get your besties, get your friends, and get that community. Don’t think that you can do this on your own because you need good nutrition, you need support, and your body is healing. You’re a human being and you’re in charge of keeping alive. It’s amazing they let you leave the hospital with a baby. They put it in this plastic thing you’ve never used but you take it out of the box and they’re like, “Bye. Don’t kill it.” After nine months of intensive reading, therapy, care, and looking at your partner going, “They let me leave with this baby. I can’t believe it.”
It is amazing. It’s important. We see the world and we think, “She makes that look easier.” How do they have a new baby? They’ve lost weight and their house is clean. The same with menopause, it’s like, “How come they stayed “skinny”?” It’s reminding people that the only way to get to your own answer is to understand what you’re navigating in the first place and you’ve got to be honest about that. We all feel some threat of something similar.
A lot of times, if you read certain Chinese medicine or whatever, keeping your cycle as long as you can can be pretty healthy in certain ways. Is there anything that we can do besides doing all these great things like getting to bed, managing our stress, and eating? Is it straight-up genetics usually about how long you keep your cycle? Is there anything we can do to prolong it?
Not that we know of yet. I met a PhD researcher who is looking at different ways to prolong the life of the ovaries because the longer your ovaries stay alive, the longer you stay alive and in better shape. The earlier you are when you go through menopause, the higher your health risks. There’s a huge genetic component, we know this. There are environmental components. The research is now starting because they’re recognizing menopause and estrogen deficiency as a pathologic state finally.

Dr. Mary Claire Haver – The rule of thumb I advise followers and patients is just to track what you’re eating for a week, eat your normal diet, and see where you’re falling.
Now we’re starting to do research. Are there things that we can do? We know we can do things that mitigate symptoms. People who eat Mediterranean diets have less dramatic menopause. The more you have hot flashes, the higher your health risks are. If you’re a super flasher, and part of that’s genetic, you have a higher risk of cardiovascular disease, meaning you have many hot flashes that are disrupting your day-to-day activities. That is something I’m curious about because the research is beginning there.
I was always interested. I still have my cycle and you wonder, “Should I be doing Chinese herbs? What should I be doing?” People are always interested in sex as they get older. People are uncomfortable talking about lubrication and things like that. She’s doing all she can and she’s feeling pretty good but sometimes it’s dryer when you’re having sex.
All women should use a lubricant and/or a moisturizer. A moisturizer is something that’s going to pull water and holds water in the vagina and keeps it moist. If you’re uncomfortable with exercise, you’re feeling some friction or rubbing on walking day-to-day activities, you would benefit from a daily moisturizer. They have high organic acid, which holds a thousand times its weight in water.
There are multiple ones on the market and they come in usually ovules or something you can insert in the vagina. They melt and they last for 3 or 4 days versus a lubricant, which is something that’s going to decrease friction. My favorite lubricants are going to be oil or oil-based or silicone-based. Astroglide is a fave at our house. My friend, Naomi Watts, makes a product called Oh My Glide. She has cute names. That is a favorite, it’s reasonably priced, and it is oil-based. K-Y makes a product called Silky. It’s vitamin E based.
Some people use plain old coconut oil and that’s absolutely fine and it works great. Watch the bacteria content on some of those packagings. There are lots of things that you do. I am a huge fan. Every woman from 35 on should be using a lubricant. 80% increase in the pleasure from orgasms with a lubricant versus not. It makes everything better down there. You need stimulation, you need a clitoral massage for most of us to have an orgasm. If that process can be easier and feel better, why not?
You’re saying even for young women.
Yeah. Try it. There’s nothing wrong with it. If it’s going to enhance your pleasure, why not? Give it a try.
I don’t know why we got uptight or weird about talking about stuff like this. Women are in this part of their life for almost 40% of their life. You talk about it. I hate when people go, “I’m that age.” They accept it. The other thing is it’s the people you’re around. All people, in general, have to be careful not to be around people that are like, “That’s how it is.” I want to encourage people to take that bull by its horns.
You have free questionnaires on your site. I would like to remind people that you said something important. You talk specifically about insulin, insulin sensitivity, and chronic inflammation. I want to remind people that exercise helps you. It’s not about burning calories, it’s about insulin management. This is something that you are clear on. There’s a great endocrinologist, Robert Lustig, who talked about, “You’re going to eat a chocolate chip cookie and think you’re going to ride your bike and burn it off. It’s ridiculous.” This whole calorie thing in and calorie out, yes, of course, you want to be aware but it doesn’t work the way people think it works.
They’re much more complicated than a bank machine.
Maybe they’ve been getting their ass kicked for a while on this and maybe they gain 35 pounds and they’re in it. There’s still a way to come back from that.
Absolutely. I see it every day.
If you’ve been feeling crazy and forgetful and all the things that everybody claims, there is a way to regain yourself. There was one interesting thing and I’ll end it on this that I did want to bring up that I thought was interesting that you talked about. If people can learn where they’re at in their health, there are some indications that hormone therapy can help with Alzheimer’s prior to it but once people have it, it may not be.
It can make it worse, Alzheimer’s and dementia. There’s a timing hypothesis for hormone replacement therapy and it’s better at prevention of these chronic diseases than at stopping it once it gets started. For the health benefits outside of hot flashes, night sweats, and sleep disruption, for the decreasing cardiovascular risk, if you already have heart disease, estrogen can make it worse for atherosclerotic disease. Starting before the disease process starts can give you a longer shelf life to live without the disease.
It’s interesting because it’s consistent. Perlmutter wrote a book, Grain Brain, and he talked about what we don’t know about Alzheimer’s because you can’t tell if your brain is chronically inflamed. Once you click over, you’re in the game and you don’t have a choice. All of these things that you’re talking about are important because while we have the chance to impact all of these things, we do that. Finally, Dr. Haver, for clarity for people on the probiotic side, you take 80 billion.
My favorite is what I picked up at the local health food store and I’ve stuck with it, The Garden of Life, 80 billion. When I’m home or traveling, I do the encapsulated because of refrigeration. Billions are better. Whatever probiotic you choose, you want something in the billions because you lose a lot in digestion. They die off from the acids in the stomach. You want enough to get through. You want something with a lot of different speciations.
Mine has, in the 30s, different species. You want some lactobacillus for vaginal and vulva health. You want streptomyces. You want all the things to help keep the gut healthy. You want to make sure that the company does some third-party testing. They have an independent tester come in to make sure what they say. These things are not regulated by the FDA. They’re considered to be food. You want to make sure that somebody has tested it to make sure that at least what they say is in it, is in it.
Do you talk about alcohol at all?
I’m going to talk about it more in my next book. Here’s the problem with alcohol. What makes alcohol healthy in the form of wine is not ethanol, it is the resveratrol in the wall of the grape. There’s a fine line in people who are enjoying a glass of wine at night. In the Mediterranean, they seem to be a little bit healthier than people who don’t do that. There’s a fine line between losing any benefit from alcohol from having too much and that’s where people struggle. It’s not the occasional drinker, it’s the people who chronically use and then abuse alcohol because of the tolerance we develop. We’ve seen a lot more of that since COVID.
Understandably. Dr. Haver, you’re a busy woman. You have practices, patients, kids, and husbands, and you’re taking care of yourself. Some people come into a world where they can navigate and deal with a lot. You seem like one of those people. Do you have a practice in place that is there to support you besides the lifestyle?
I’ll give you an example. Even though I tend to be what someone would say is more Stoic, you come from an athletic background, you go into a medical school, and a big family. You probably just deal with it. I do always check in to see how I’m feeling. Genuinely, I’m pretty good about standing up for that. I do that one thing. Is there something you do that helps you because you do manage much that helps you keep the decks clear?
I worked with a therapist for a while. This is probably the best thing I’ve ever done. What she got me practicing were meditation and journaling. Those were things that I felt were woo-woo and wouldn’t be helpful. In yoga, I’m like, “What’s she doing? Is that a bug?” I’m like, “There’s no way I’ll be able to meditate.” I downloaded this app at her suggestion called Headspace and did guided meditation for 3 or 5 minutes, nothing crazy. I was astounded by that. I could do it and I look forward to it and I enjoy it.
For journaling, it’s mostly gratitude, taking a minute to say thanks to the world for my life. What am I letting go of today? The things that I’m letting get under my skin or bother me, imagining in my head, and writing them down. It’s people. I wrap it in a bubble or a balloon and then I let it go into the sky and I see it floating away. That’s my visual imagery of things that are bugging me. Being consistent with that practice helps me be a better person and better serve my community.
[bctt tweet=”See how you feel. Do your workouts. How are you feeling? Listen to your body.”]
Is there something that showed up to be true for you to help you in parenting? I always talk about being an example. Trying to simplify it. Is there anything that showed up for you being a parent that supported what you were trying to accomplish as a parent?
It was the meditation and journaling and then watching my children turn into adults and going from that relationship change of hovering and having to manage to watching them become people and making their own decisions. I have cranked out two magnificent human beings. My husband, our community, our friends, and our extended family have all helped them be wonderful people.
Did I screw it up? Absolutely. Are there things I regret? Yes. I checked out after my brother’s death. I can’t even tell you what they did during those six months but they survived. Trying to set an example of being able to manage all the things and saying no and setting up boundaries has been the best parenting lesson. teaching them that it’s okay to set boundaries and say no. You have to protect you first. That next layer, which is your kid, the people who you bring into that first circle, and keeping those things a priority is something I did not do well when they were little. I said yes to everything. I wanted to be supermom and super doctor and super whatever.
Menopause has been helpful there. My give-a-shit factor has decreased and I’m focused on what works for me. I can let go that they’re going to be okay. I don’t have to worry about them. I do worry, of course. I’m a mom. I’m not checking their location every five minutes when they’re out at the bars. They are making good decisions and I can relax and rest and focus on me.
Finally, in marriage, what showed up for you? You have been in a long relationship and you guys are busy and you’re two different individuals creating this family. What were things that kept coming and throwing up that helped both of you navigate the relationship or you? We come in one way and then we get the skillset and we go, “That seems to work.”
We never wanted to break up at the same time. I don’t know if that is luck or whatever. Whenever one of us was pulling away, the other one was hanging in there. I’ve found a new voice through this process and being able to verbalize what I need. He’s happy. He could stay doing the same thing forever. He’s a good person all the time. The only thing he gets upset about is the house is messy because he’s type A like that. It might take him a minute, “Listen to what I’m saying and internalize it.”
He wants to be a person that I can count on. I don’t want to say make me happy like that. Realizing that I have a voice and I can verbalize the things that I want. We’ve gone from a marriage to a partnership. We’re at a point where don’t have to stay together because the kids are fine. Financially, we’ve both done okay. We’re not tied to each other because of that either. Now we’re deciding to be together and grow old together and it’s exciting. We’re going to Patagonia for two weeks to go hiking.
Did I miss something that felt important and that I didn’t cover that you want to remind people about before we go?
The top tip that I can give people that you’re probably not doing, at least as far as nutrition goes, is to make sure you’re getting enough fiber. Track it for a couple of weeks and then try to add foods. Take a Vitamin D supplement. Ask your doctor to have your levels checked, most of them will do it. You may need a much higher dose than you think. Get your sunshine and eat your salmon if you can as good sources but you’re probably going to need a vitamin D supplement.
Aging is normal but suffering is not. All of us expect to not feel the same as we did at 25. If you are life disruptive and you are not happy because of how you feel, you need to find the right person to guide you through this. You do not have to suffer through this. You can be a whole person feeling normal, feeling productive, and having the best years of your life right now.
Dr. Haver, can you remind everybody of all the places where they can find you? Thank you.
Our website is GalvestonDiet.com. You can find me on TikTok, @DrMaryClaire, and also on Instagram. We’re on Facebook and YouTube. My YouTube channel has longer videos where I do a lot of talk around menopause and nutrition. We’re also on Pinterest. Pretty much everywhere. If you go to our website, you can click all the social media channels there.
I appreciate what you are reminding people and consolidating all the information. Congratulations on this next chapter. I’m excited for you. It’s like a bolt-on to what you were already doing and now being able to bring that to more people. Thank you and thank you for your time.
You’re welcome.
—
Thank you so much for reading this episode. Stay tuned for a bonus episode where I go deeper into one of the topics that resonated with me. If you have any questions for my guest or even myself, please send them to @GabbyReece on Instagram. If you feel inspired, please hit the follow button, and leave a rating and a comment. It not only helps me, it helps the show grow and reach new readers.
Subscribe to The Gabby Reece Show
[podcast_subscribe id=”5950″]
Resources mentioned:
- The Galveston Diet
- Dr. Gabrielle Lyon – past episode
- Dr. Stacy Sims – past episode
- Midi Health
- Evernow
- My Alloy
- Grain Brain
- GalvestonDiet.com
- @DrMaryClaire – TikTok
- Instagram – @DrMaryClaire
- YouTube
- @GabbyReece
About Dr. Mary Claire Haver
 Dr. Mary Claire Haver is a wife, mom, physician, and entrepreneur who has devoted her adult life to women’s health. As a Board Certified OBGYN near Houston, Dr. Haver delivered thousands of babies, completed thousands of well-woman exams, counseled patients, taught residents, and did everything an academic professor and OBGYN could do. As her patient population aged, Dr. Haver was overwhelmed with the number of complaints and concerns her patients had with weight gain while going through menopause. For years, she told her patients to eat less and exercise more. It wasn’t until she, too, experienced the changes of menopause and mid-life weight gain that she realized this advice didn’t work and ultimately led to her creating and developing her online program, The Galveston Diet, which currently has over 100,000 students. The book version of The Galveston Diet was released by Penguin Random House in January 2023. The Galveston Diet helps women reach their health and wellness goals through an anti- inflammatory approach to nutrition. Dr. Haver believes in the power of nutrition and anti-inflammatory foods to combat midlife inflammation and highly recommends the unique benefits of intermittent fasting.
Dr. Mary Claire Haver is a wife, mom, physician, and entrepreneur who has devoted her adult life to women’s health. As a Board Certified OBGYN near Houston, Dr. Haver delivered thousands of babies, completed thousands of well-woman exams, counseled patients, taught residents, and did everything an academic professor and OBGYN could do. As her patient population aged, Dr. Haver was overwhelmed with the number of complaints and concerns her patients had with weight gain while going through menopause. For years, she told her patients to eat less and exercise more. It wasn’t until she, too, experienced the changes of menopause and mid-life weight gain that she realized this advice didn’t work and ultimately led to her creating and developing her online program, The Galveston Diet, which currently has over 100,000 students. The book version of The Galveston Diet was released by Penguin Random House in January 2023. The Galveston Diet helps women reach their health and wellness goals through an anti- inflammatory approach to nutrition. Dr. Haver believes in the power of nutrition and anti-inflammatory foods to combat midlife inflammation and highly recommends the unique benefits of intermittent fasting.